How to Get Rid of Allergies
It’s so common to have allergies these days that no one bats an eye when they hear about environmental, food, or chemical allergies. The alarming thing is that allergies are actually a modern-day disease with numbers growing dramatically in the last century alone. It’s estimated that 30%-40% of people worldwide have some form of allergy. Most people take this at face value and don’t question their allergy’s root cause. This is probably because we’ve been continually sold the idea that all antihistamine medications are safe and they are the best way to manage these health issues long-term. However, there are always consequences and side effects with all medication.
What if we told you that many allergies are actually reversible with root-cause treatment? Let’s take a closer look at the root causes of allergies, the problems with antihistamine medications, and how to finally stop allergies from inhibiting daily activities.
What Is an Allergy?
An allergy is an abnormal immune system reaction to a foreign substance. The immune system recognizes this substance as harmful, leading to an allergic reaction. Allergic reactions are characterized by the symptoms experienced. Allergy symptoms can range from mild to life-threatening and are very bio-individual.
The most common allergens include:
- Pollen
- Animal dander
- Dust mites
- Insect stings
- Mold
- Food
- Latex
- Medication
- Cockroaches
The Types of Allergic Reactions
There are four categories of allergic reactions recognized by allergists:
- Type I | Anaphylactic Reactions: Type I reactions are the most common allergic response and are often triggered by animal dander, pollen, certain foods, and dust mites. With this type of reaction, your body releases histamine and other chemicals that induce inflammation and swelling throughout the body. Symptoms of this reaction type include itching, hives, and anaphylaxis with food; eczema or rashes with skin reactions; runny nose, itchy eyes, congestion, and asthma with inhaled allergens.
- Type II | Cytotoxic Reactions: Type II reactions happen when IgG or IgM antibodies bind with antigens on the surfaces of cells. The chain reaction damages cells by activating a component of immunity called the complement system. Symptoms tend to happen within minutes or hours of exposure to the allergen. This leads to conditions such as autoimmune neutropenia, autoimmune hemolytic anemia, immune thrombocytopenia, Grave’s disease, Goodpasture syndrome, and Myasthenia gravis.
- Type III | Immunocomplex Reactions: Type III reactions are also associated with IgG and IgM antibodies. When these antibodies are bound with antigens, they can form immunocomplexes that settle on tissues and organs. As the body attempts to remove these immunocomplexes, it damages the underlying tissue. Symptoms generally occur several hours after exposure. This leads to conditions such as lupus, rheumatoid arthritis, Arthus reaction, and serum sickness.
- Type IV | Cell-Mediated Reactions: Type IV reactions, also known as delayed allergic reactions, take at least 24 hours after exposure to an allergen before symptoms manifest. They most commonly happen around 48-72 hours after exposure. Symptoms of this reaction type include chronic asthma, fungal infections, tuberculin reactions, and contact dermatitis.
Understanding the Difference Between Allergies, Sensitivities, and Intolerances
You’ve probably heard of the terms sensitivities and intolerances. They are actually different than allergies– here’s how each of these terms is characterized:
- Allergy: Although this word is commonly used to describe poor reactions to foods, drugs, and chemicals, and synonymously with sensitivities and intolerances, a true allergy is an immune reaction to a substance.
- Sensitivity: A sensitivity doesn’t involve an immune response. It is characterized as a reaction to a substance– the reaction is an exaggeration of a normal side effect and is often delayed. While it doesn’t cause an immune system response, sensitivities can lead to multiple symptom reactivity ranging from GI issues to neurological problems. Some issues that are associated with sensitivities can be life-threatening, especially if that person is repeatedly exposed to that substance.
- Intolerance: An intolerance is characterized as the body lacking a chemical or enzyme needed to digest a certain food. Since the digestive system doesn’t produce sufficient quantities of a specific enzyme or chemical needed to break down that food, symptoms occur. An example of a common intolerance is lactose intolerance, the inability to digest the sugar (lactose) in dairy.
Sensitivities and intolerances do not involve the immune system and are more common than allergies.
IgE vs. IgG
Regarding food sensitivities and allergies, you may have heard about food sensitivity tests. These tests look for an IgG reaction while allergy tests look for an IgE reaction. Even though IgE food allergy tests are accurate for identifying true allergies, there are many issues when it comes to IgG food sensitivity tests. The IgG test can sound compelling, featuring up to 100 foods with a single panel. Aside from breath tests used to gauge intolerances, food sensitivity tests have never been scientifically proven. The only way to figure out food sensitivities is by tracking symptoms while utilizing an elimination diet such as the Carnivore Cure elimination diet. The antibodies measured in IgG tests are produced as a part of the immune system’s response to foods and haven’t been shown to correlate with either symptoms or intolerances.
What Causes Allergies, Sensitivities, and Intolerances?
Did you know that no one is born with an allergy? Allergies, sensitivities, and intolerances develop at any point in a person’s life once the immune system comes into contact with the substance. Genetics can play a factor– if a parent is allergic to a certain substance, there’s a 50% chance that you may develop that allergy. If both your parents are allergic to that substance, the risk for you goes up to 75%. However, it’s important to note that genetics are never destiny. Many other factors come into play such as your environment, diet, and even stress.
Allergies and Autoimmunity
Allergies and autoimmunity are both conditions that result from an inappropriate immune response. Another similarity shared between the two is the pathway of development involving immune cells in the immune response. With allergies, the immune system reacts to harmless allergens leading to the activation of immune cells. With autoimmune disease, immune cells often recognize self-tissues as foreign, activating immune cells that result in tissue damage and inflammation. Both allergies and autoimmunity share common triggers such as environment, diet, and stress. Some studies have found that individuals with autoimmunity may have an increased risk of developing allergies and vice versa. While the relationship between allergies and autoimmunity is very complex and bio-individual, both conditions are tied to the immune system.
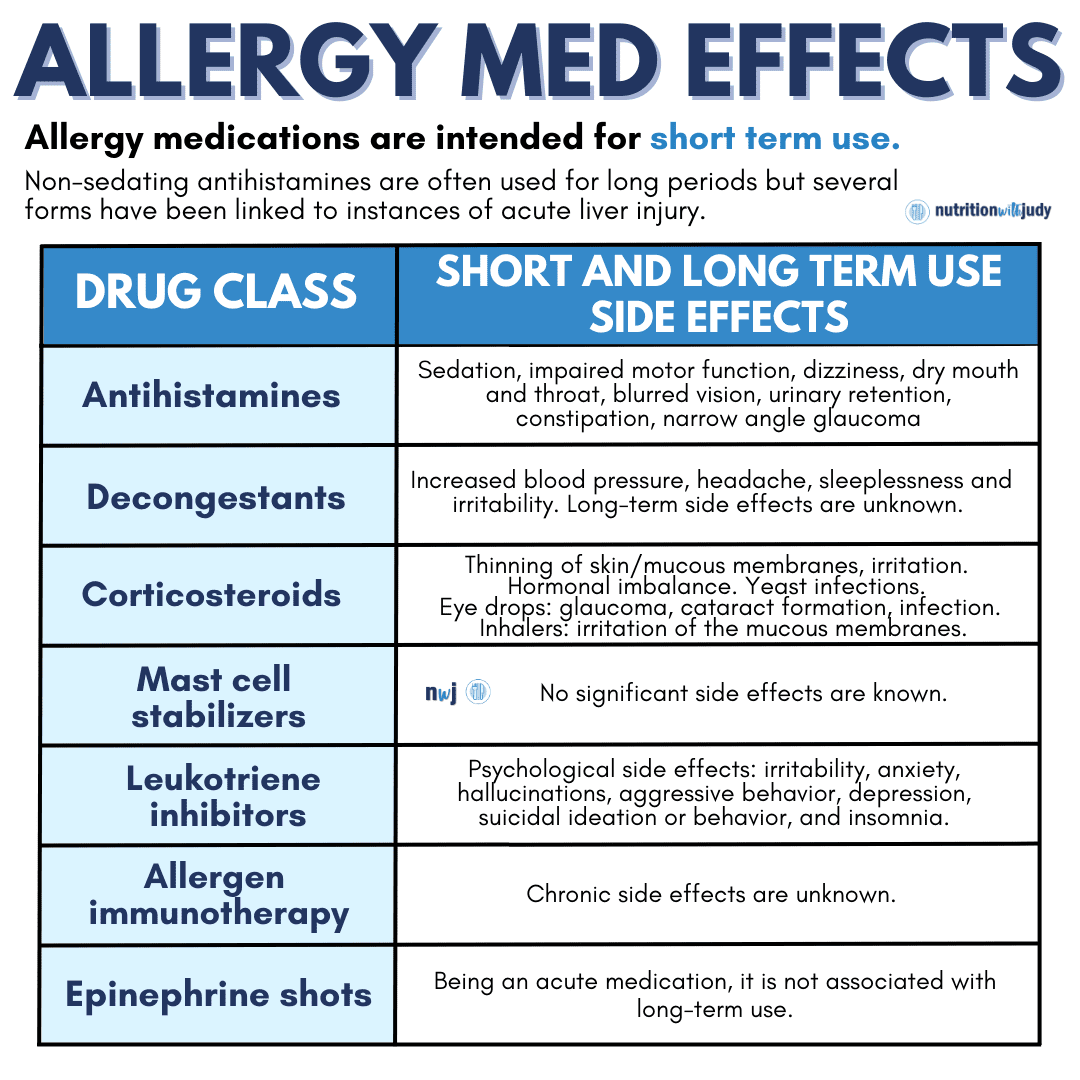
Why Allergy Medication Isn’t Ideal
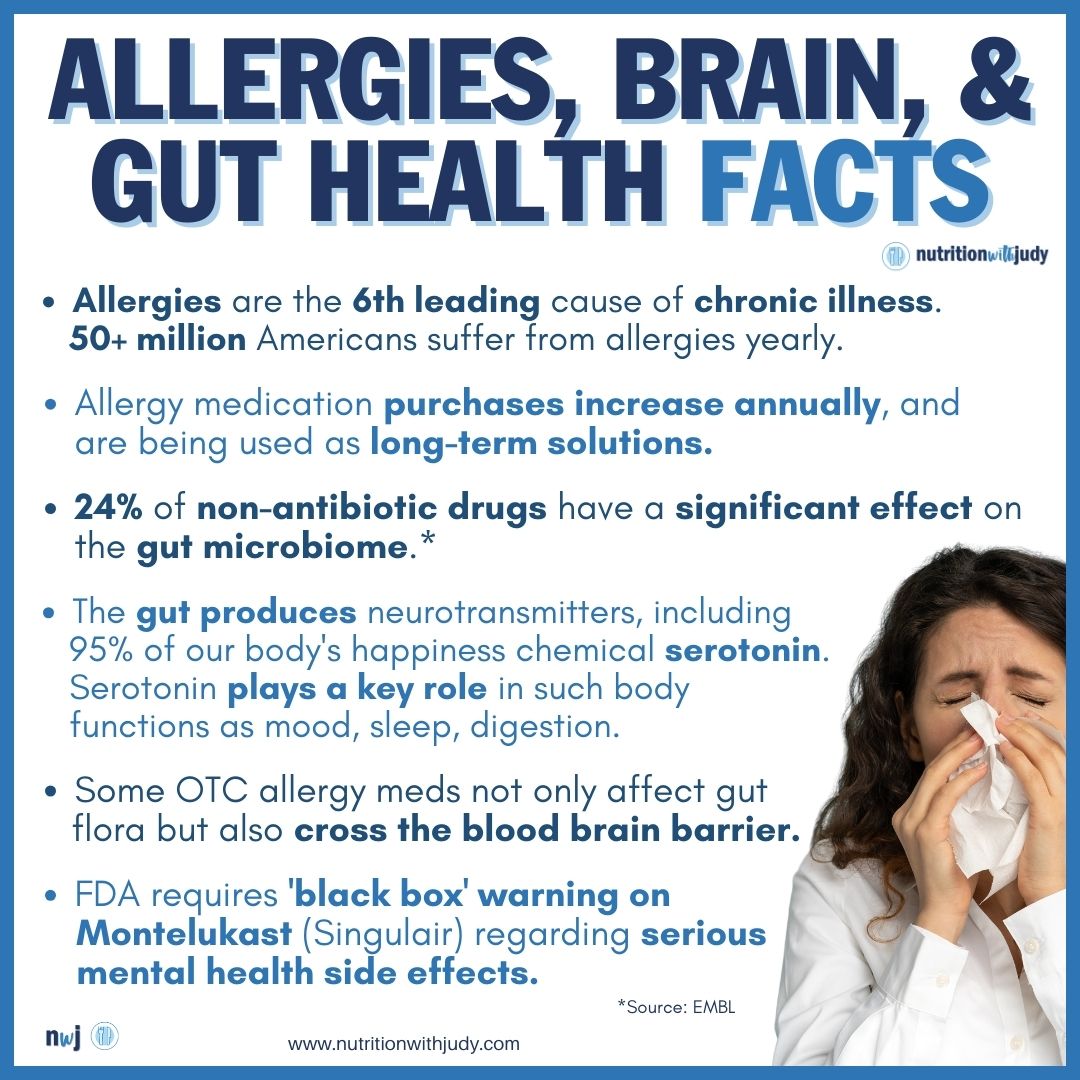
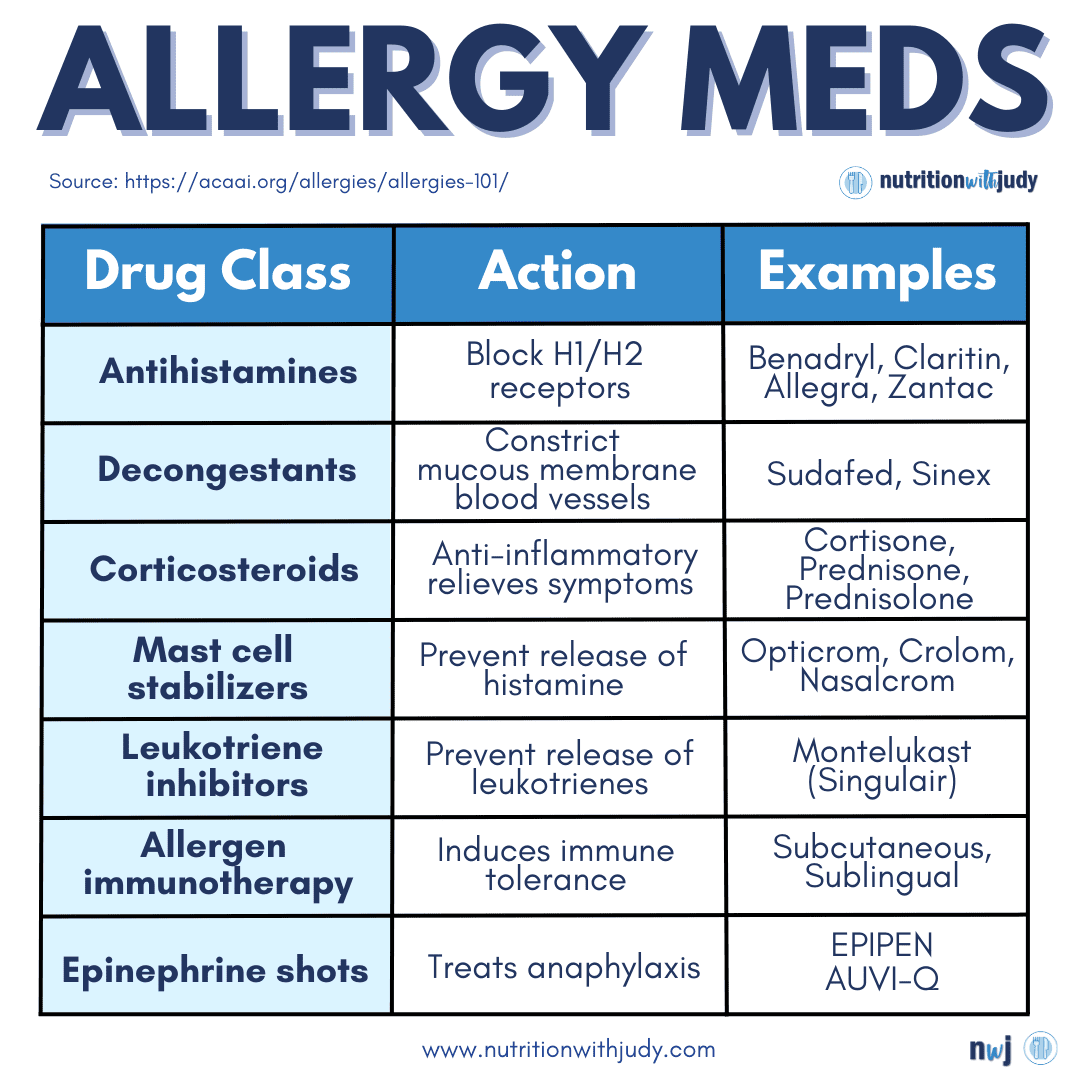
The CDC has classified allergies as the sixth leading cause of chronic illness in the US, costing over $18 million annually. These medications are meant for short-term use but have become long-term crutches for most people. The long-term overuse of drugs has a negative impact on our gut and psychological health, leading to more problems and the continuation of the allergies we’re trying to alleviate. Antihistamine medications only block histamine receptors and don’t actually reduce histamine levels.
The long-term use of first-generation antihistamines such as Benadryl increases the risk of dementia and cognitive decline. First-generation H1 and H2 antihistamines can also impair the innate immune response to bacteria. Second-generation antihistamines can be safer but still adversely impact the gut microbiome and lining, causing allergies to persist. Due to the gut-brain axis, impacted gut function ultimately affects our mental health as our serotonin levels drop.
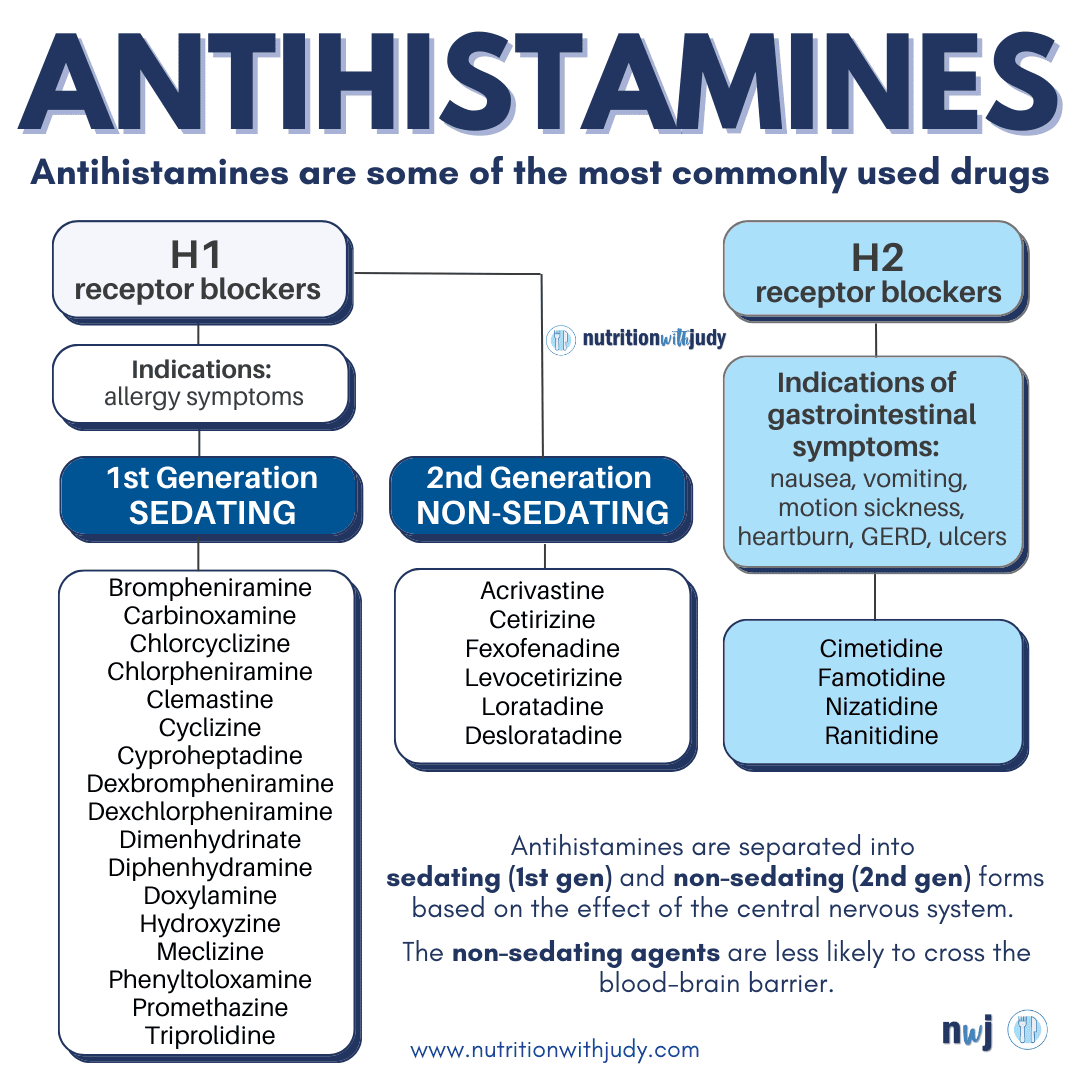
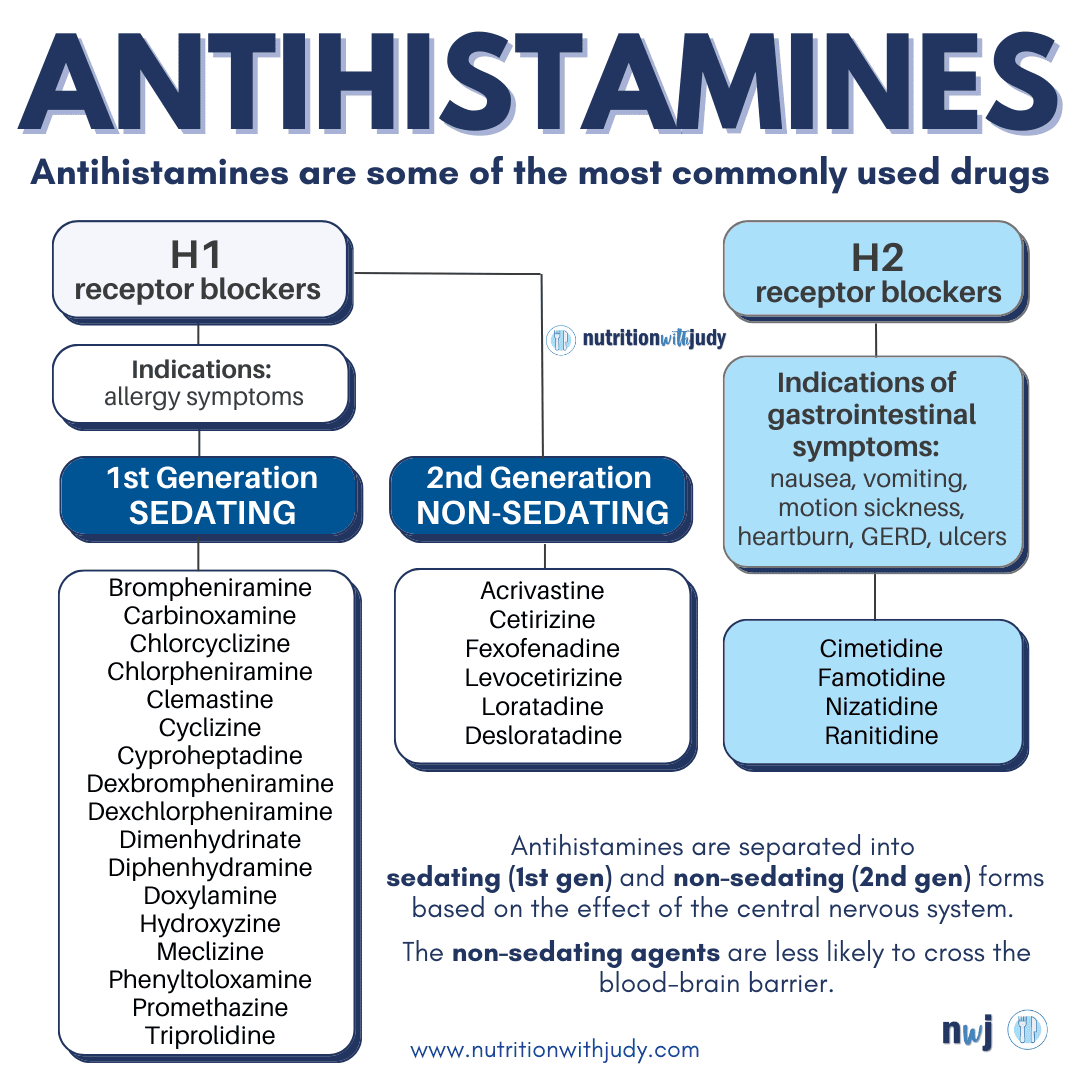
H2 antihistamines lower the gut’s histamines by blocking stomach acid production. Stomach acid is needed for proper food digestion, nutrient absorption, and killing pathogens such as bacteria, viruses, mold, and parasites. Without adequate stomach acid levels, this can lead to intestinal infections including SIFO and SIBO, acid reflux, low neurotransmitters, and nutrient malabsorption.


Serious neuropsychiatric (NP) events have also been reported with the use of the antihistamine Singulair (montelukast). These events include suicidal ideations and behavior, suicide, depression, and obsessive-compulsive symptoms. The CDC has since issued a Singulair black box warning because of these serious mood-related symptoms.
Not only does the body develop a tolerance to antihistamines over time, but certain antihistamines that include diphenhydramine, cimetidine, or promethazine actually block diamine oxidase (DAO) production. DAO is an enzyme that the body makes in order to break down histamines from food. A DAO deficiency can contribute to or worsen histamine intolerance. Histamine intolerance develops from too much histamine in the body, leading to multi-system symptoms ranging from GI issues to neurological reactions.
The Connection Between Allergies and Gut Health
Between 60 and 70 million Americans suffer from gut disease. As a result, the number of people suffering from allergies is on the rise. When we begin to heal our gut, we address the actual cause of our allergies. The best defense against allergies lies within the gut. Remember, 70% to 80% of the immune system is in the gut. If you have allergies, sensitivities, and/or intolerances, it’s a sign your immune system is inundated with noise.
Research supports the connection between food and environmental allergies with gut health. Here are some studies showing the link between food allergies and gut health:
- Immune system dysregulation within the intestines linked to allergies
- Enzyme deficiencies can lead to food intolerance
- Leaky gut increases the risk of allergies
- Bacterial overgrowth such as SIBO can lead to food sensitivities
- Gut infections including SIFO and parasites can lead to food sensitivities
- Infant gut dysbiosis may be linked to childhood food allergies
- Reduced healthy bacteria in the microbiome
Here’s the data showcasing the link between seasonal allergies and gut health:
- Higher rates of seasonal allergies in adults with lower levels of butyrate-producing bacteria
- Many GI disorders including IBD, GERD, gastritis, IBS, peptic ulcers, gastroenteritis, constipation, and colitis are associated with an increased risk of seasonal allergies
- People with seasonal allergies and asthma are more likely to have GI symptoms
Treating the gut is often the first line of defense for many conditions and is a root-cause approach for allergy, sensitivity, and intolerance treatment.
Root-Cause Healing for Allergies, Sensitivities, and Intolerances
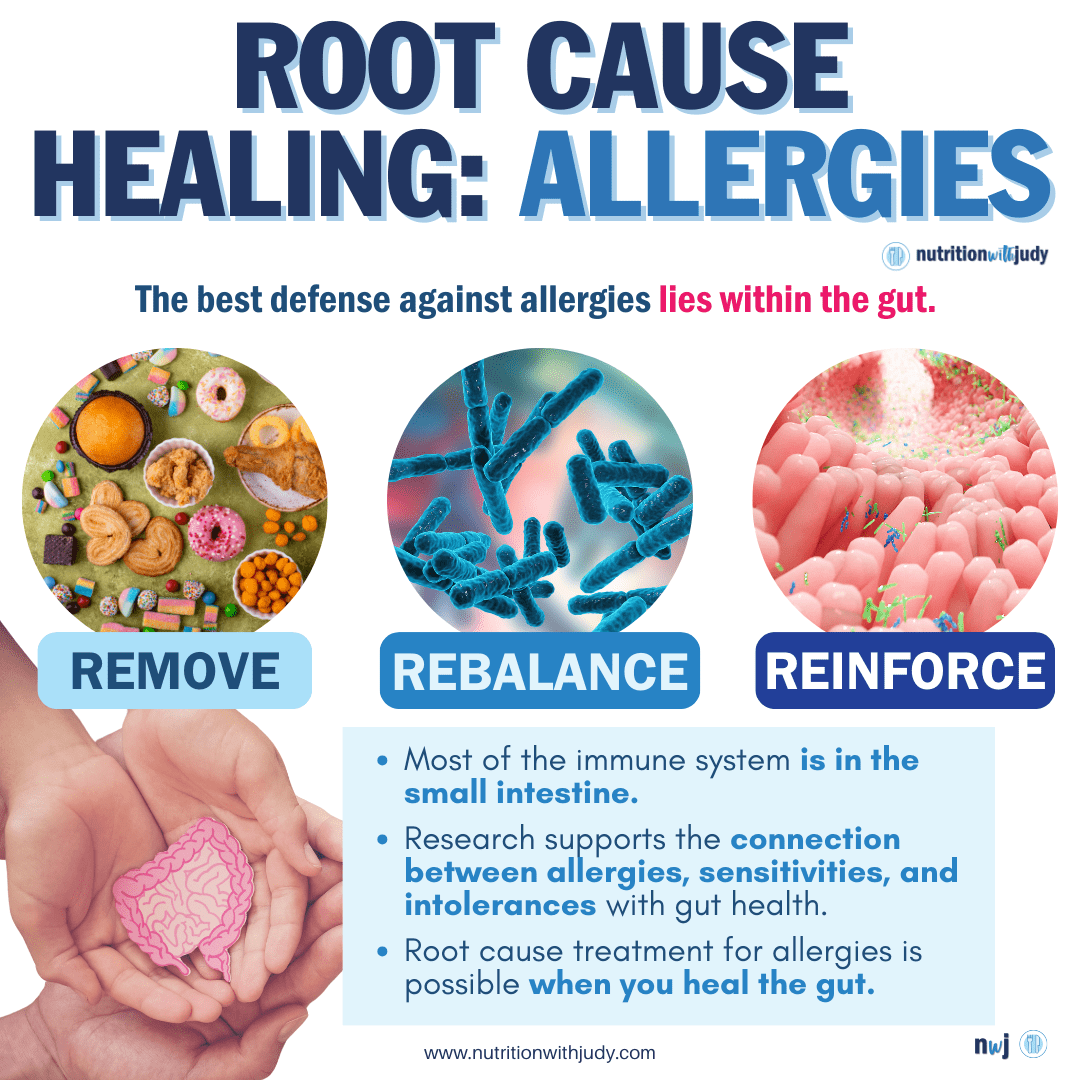
Addressing the root cause of our allergies is the safest and most effective solution. Healing the gut requires a three-pronged comprehensive approach that includes the steps of remove, rebalance, and replace– you can read more about gut healing here.
The Carnivore Diet for Allergies
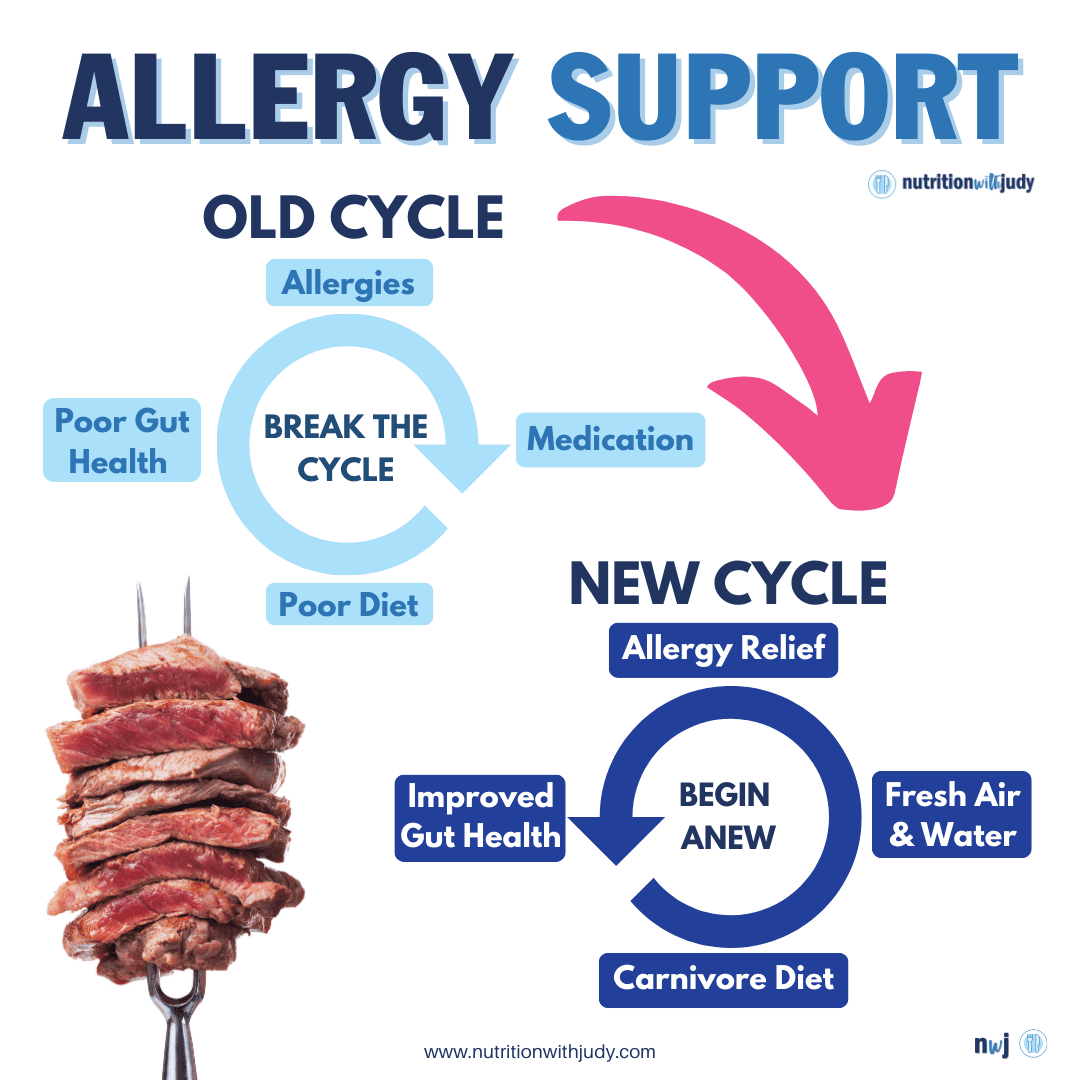
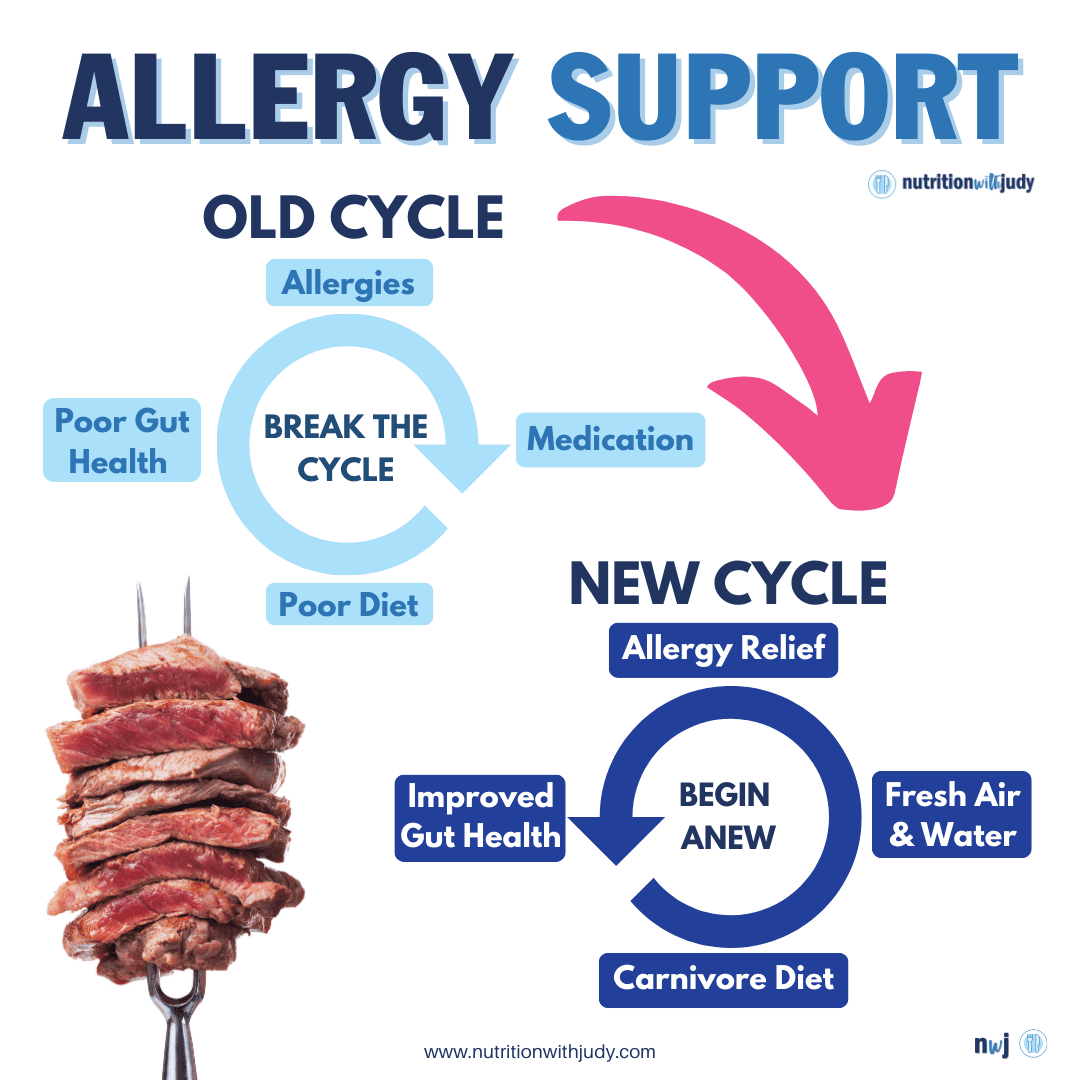
The Carnivore Cure elimination diet leverages the powerful carnivore diet for optimal gut healing and support. This is a great place to start for those interested in root-cause allergy healing. In our clinical practice with over 1,500 meat-based clients, individuals often report a significant reduction in allergies, sensitivities, and intolerances. Since gut conditions such as leaky gut, bacterial overgrowth, and gut infections can contribute to the development of allergies and sensitivities, the carnivore diet is the ultimate dietary tool for helping support and heal these conditions.
Probiotics for Allergies, Mast Cell Activation, and Gut Health
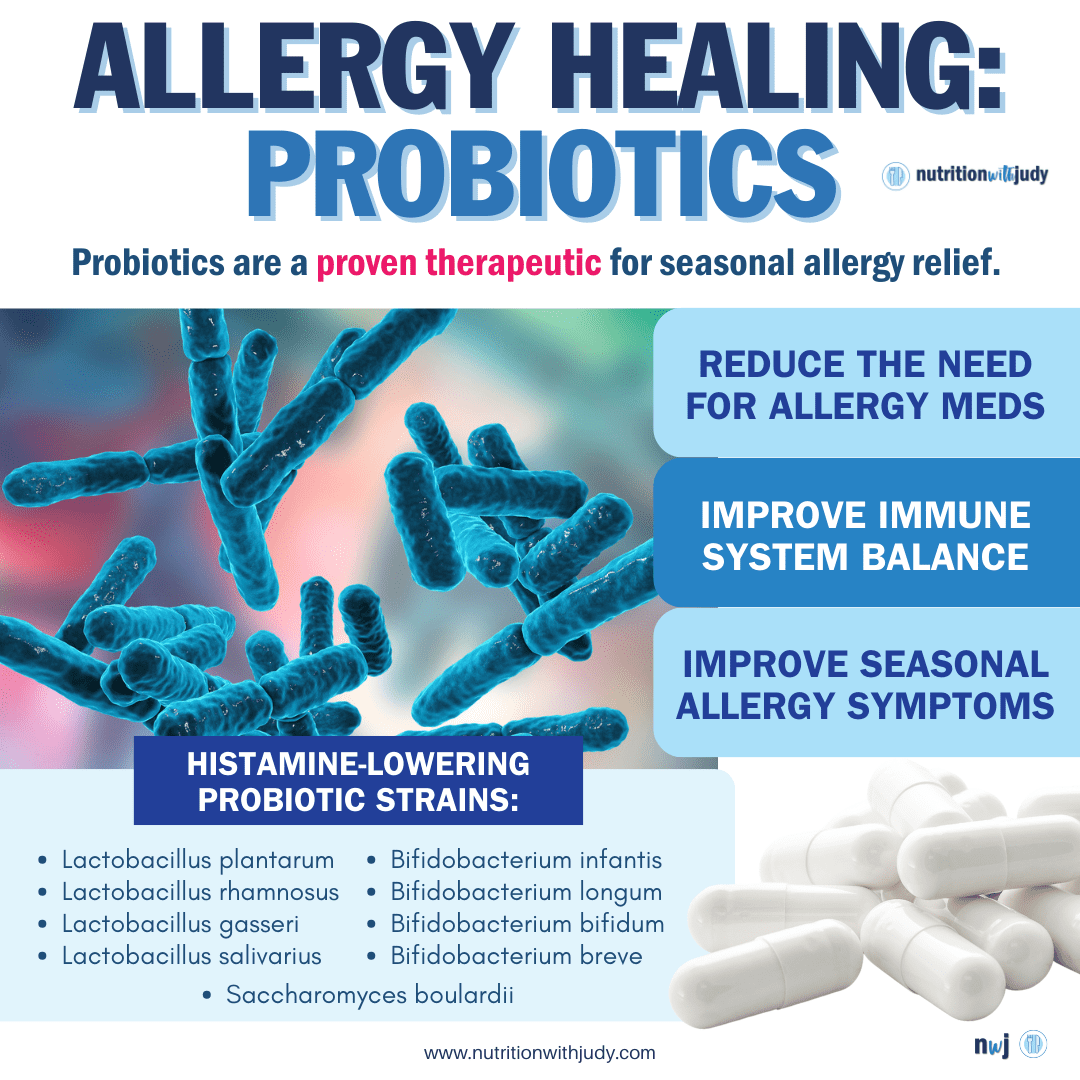
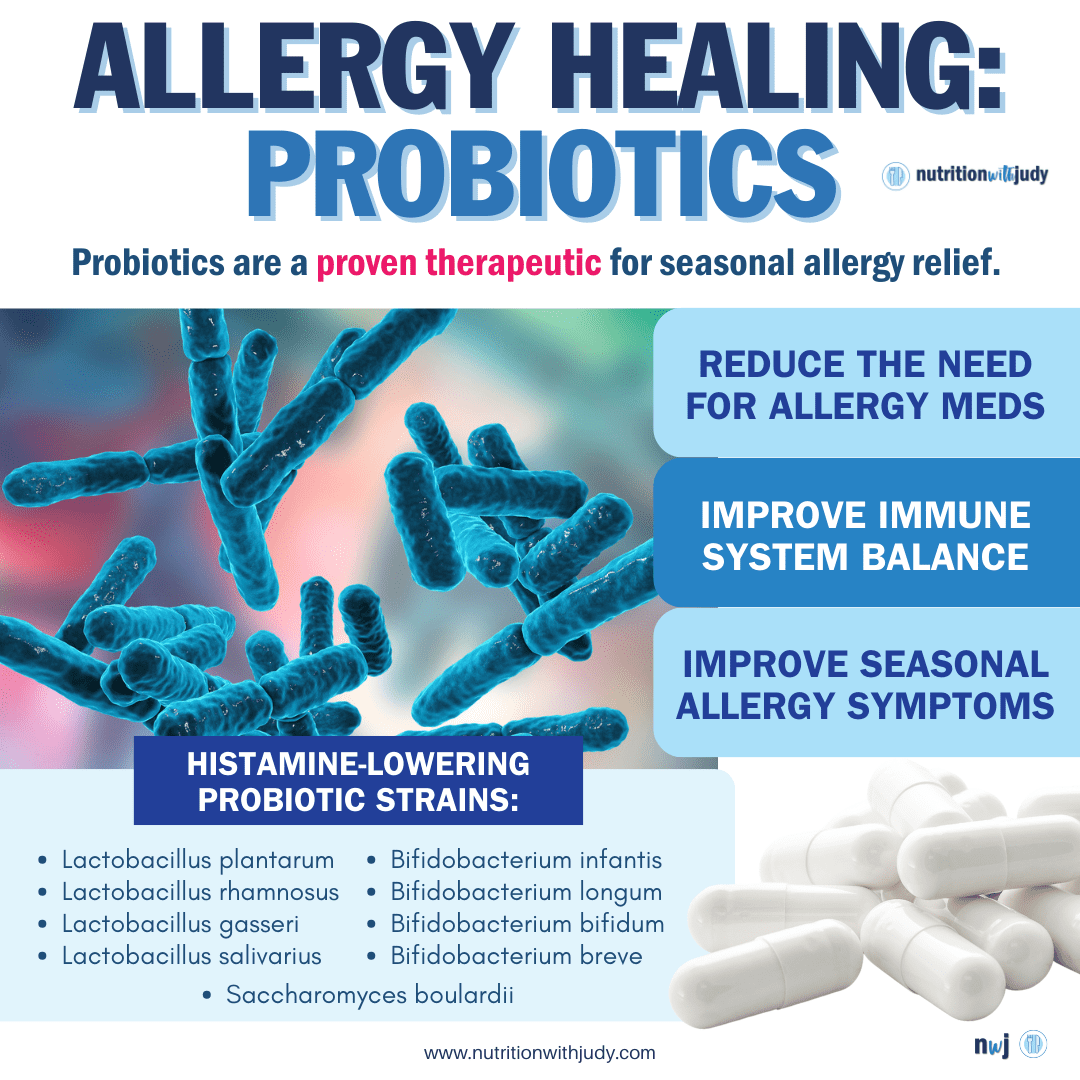
Probiotics are often utilized in gut healing protocols and are a proven therapeutic for seasonal allergy relief. One study found that probiotics reduced the need for allergy medication. Another review reported that probiotics significantly improved seasonal allergy symptoms in addition to enhanced immune system balance.
Certain probiotic strains can help lower histamine levels. It’s important to note that if you suffer from histamine intolerance, mast cell activation syndrome, or other histamine issues, there are probiotic strains that increase histamine levels in the gut.
Mast cell activation syndrome (MCAS) is a condition that involves a faulty activation of mast cells— mast cells are the blood cells that are part of the immune system. Mast cells play a critical role in the immune system’s response to allergens and pathogens, as they release substances such as histamines in response to triggers. This is a very rare root-cause condition– most people suffering from mast cell issues or histamine intolerance are generally experiencing this as a symptom of a deeper root cause. That means if you’re experiencing any mast cell or histamine issues, we highly recommend looking deeper at conditions such as gut dysbiosis and environmental illness.
If you suffer from mast cell activation, mast cells are hypersensitive and become activated too easily and frequently. This excessive activation leads to a variety of symptoms that resemble allergic reactions. These symptoms affect all multiple organ systems, including the skin, GI tract, cardiovascular system, respiratory system, and more.
If you suffer from histamine issues or SIBO, soil-based probiotics are generally better tolerated. Always work with your trusted practitioner to find the right probiotic options for you. However, specific Lactobacillus and Bifidobacterium have been shown to reduce histamine levels which in turn could help with lowering allergy symptoms. The probiotic yeast strain Saccharomyces boulardii has been shown to increase DAO production in animal models, which may help naturally break down histamines in the gut. You can find our favorite probiotic supplement with S. boulardii here.
Research also suggests that probiotics may help improve lactose intolerance symptoms. A randomized controlled trial found that probiotics combined with an elimination diet improved lactose intolerance symptoms better than diet alone. Another study reported that probiotic use was associated with considerable improvements in digestion and lactose intolerance symptoms.
The Role of Butyrate
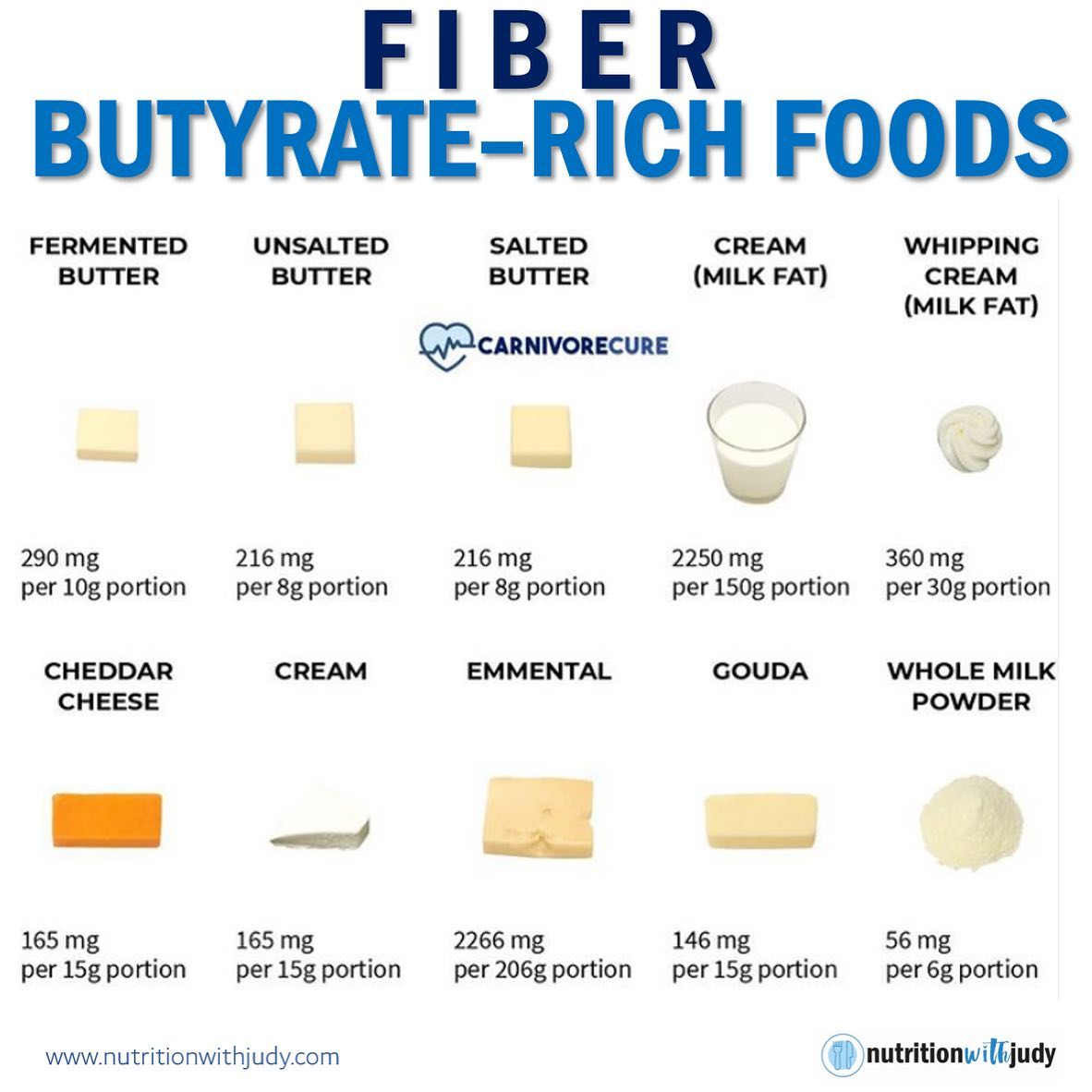
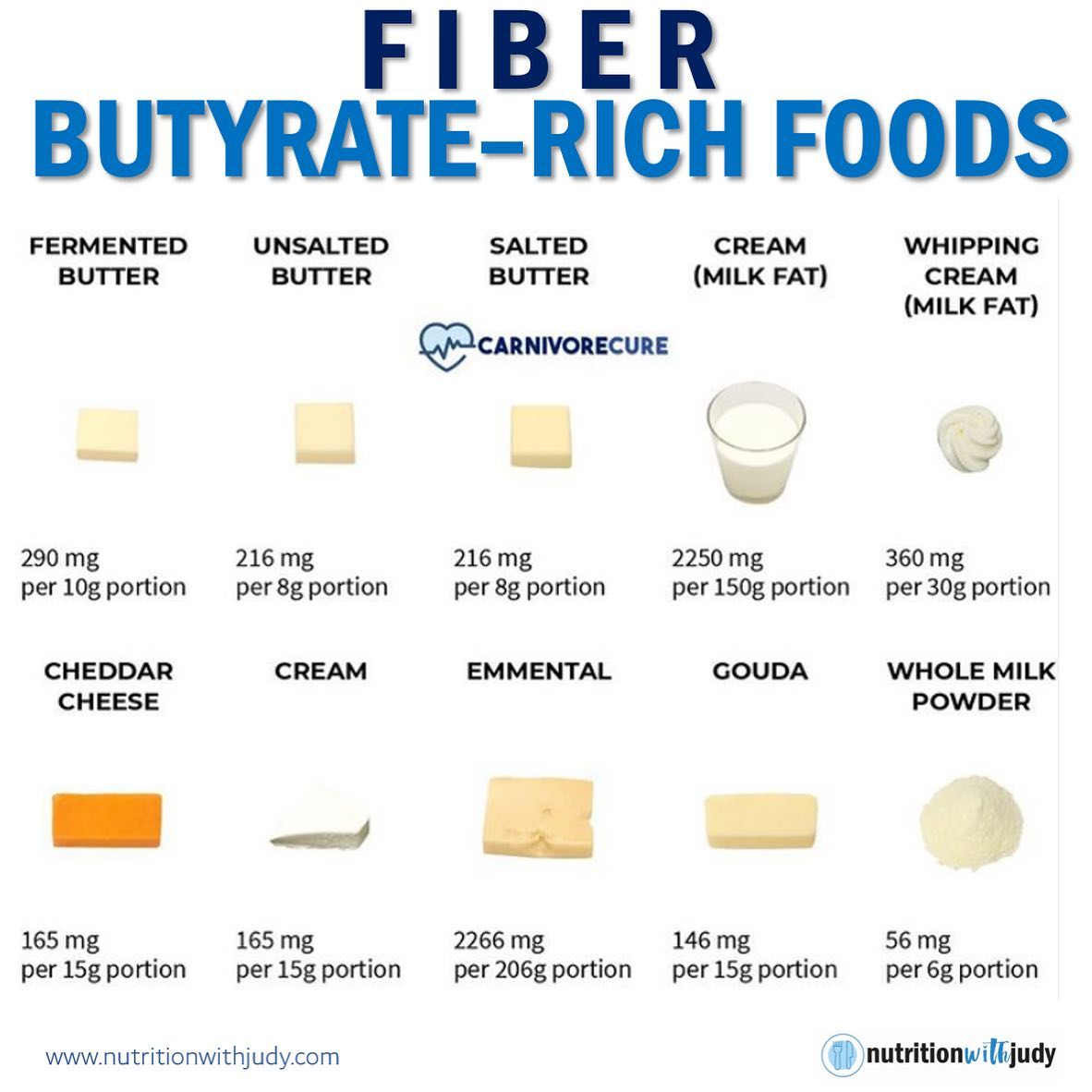
Butyrate is a short-chain fatty acid that plays an important role in digestive health. It’s the main energy source for colon cells, supports the immune system, reduces inflammation, and promotes a healthy gut barrier. While there’s a common misconception that butyrate is best obtained from fiber-rich foods, butter and other dairy products are actually an even better source and don’t have all the disadvantages that come from plant foods.
Researchers are currently investigating the potential therapeutic value of butyrate supplementation for reversing food allergies. As mentioned above, one study found that individuals with lower butyrate levels had higher rates of seasonal allergies, so this could prove beneficial. Stay tuned as more animal research and clinical trials on butyrate supplementation for food allergies are on their way.
Closing Thoughts
While some severe food allergies leading to life-threatening anaphylaxis may not be reversible, we’ve had incredible improvements and reversals with various food, environmental, and chemical allergies, sensitivities, and intolerances in our clinical practice. Root-cause healing is possible for allergies. Focus on utilizing a powerful anti-inflammatory diet such as the carnivore diet and a comprehensive gut healing protocol for alleviating allergy symptoms. Antihistamines are never root-cause treatment, only a bandaid. And remember– if your gut doesn’t heal on a carnivore diet, consider environmental illnesses such as Chronic Inflammatory Response Syndrome (CIRS) that may be plugging up your immune system.
Work With Our Trusted Carnivore Diet Functional Nutritional Therapy Practitioners
The Nutrition with Judy practice is honored to be a trusted carnivore diet practitioner support serving clients from around the globe. We’re passionate about helping our clients achieve root-cause healing in order to lead the best quality of life possible that’s nearly symptom-free. Our team is dedicated to educating our community about the incredible benefits of the carnivore diet. We welcome you to explore our free resources and are always available to support you through personalized protocols. Our Symptom Burden Assessment (SBA) is the perfect starting point for discovering your root cause and is required to work with our team— you can learn more in-depth about this powerful tool here.
Start your root-cause healing journey today and contact us any time with any questions or concerns.
DISCLAIMER: This content is for educational purposes only. While we are board-certified in holistic nutrition and are nutritional therapy practitioners, we are not providing medical advice. Whenever you start a new diet or protocol, always consult with your trusted practitioner first.


Deanne Hislop
December 4, 2023 at 7:08 pmThis is so interesting in terms of butyrate as dairy is typically reduced in atopic type individuals. While there are so many things at play with allergies, it is interesting that there has been both a trend in reducing dairy (full fat dairy) and an increase in allergies. I am assuming that skim milk is a poor source of butyrate?