

Understanding SIFO and How to Treat It


Having optimal gut health is essential and provides the foundation for overall wellness. Impacted gut health often plays a significant role in a variety of chronic illnesses and can even be a root cause of certain conditions ranging from mental health to autoimmunity. Since our practice specializes in root-cause healing, gut healing is always at the forefront of our approach. Many individuals, including all of our clients and patients, decide to try the carnivore diet for supporting gut health and healing their gut dysbiosis and gastrointestinal (GI) conditions. While the carnivore diet can offer robust support for many gut issues, certain conditions will require treatment through a specialized, often personalized protocol.
A less commonly known gut condition that could be causing your unexplained GI symptoms is small intestinal fungal overgrowth, also known as SIFO. SIFO is a new discovery in mainstream health, with the first published research paper released in 2015. As with any new discoveries in the medical space, there can be skeptics and more research is needed. Here’s what we do know about SIFO and the importance of following a proper treatment protocol for eradicating this fungal infection.
What Is SIFO?
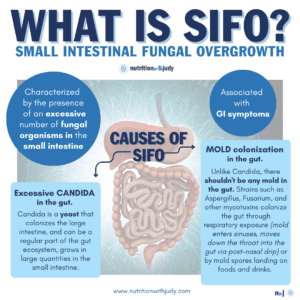
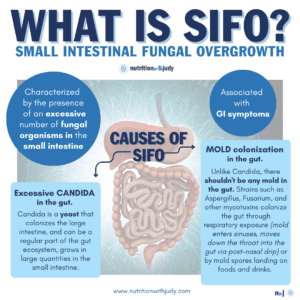
While some fungal strains, similar to bacterial strains, can be a regular part of the gut ecosystem and mostly colonize the large intestine with minimal colonization in the small intestine, problems happen once there is heavier colonization in the small intestine that leads to overgrowth. SIFO is characterized by the presence of an excessive number of fungal organisms in the small intestine associated with GI symptoms. Essentially, SIFO occurs when yeast, also known as Candida, grows in large quantities in the small intestine. This can sometimes be referred to as chronic candidiasis or yeast syndrome. Candidiasis is known to cause GI symptoms, particularly in immunocompromised patients or those taking antibiotics or steroids. With Candida overgrowth, it can be common to experience other bodily symptoms including vaginal yeast infections, white coating on the tongue, sinus congestion, postnasal drip, as well as bad sugar and carbohydrate cravings.
However, candida can be only part of the problem. Another culprit behind SIFO is mold colonization in the gut. Typically, the recommendation for Candida is to starve the yeast by eliminating all sugars including fructose from fruit– but when this doesn’t resolve on a carnivore diet, we need to consider SIFO from mold colonization. Those with SIFO from other types of fungal species won’t recover from only addressing Candida. Unlike Candida, there shouldn’t be any mold colonized in the gut at all. Certain molds such as Aspergillus or Fusarium are types of fungi that can colonize the gut and also cause SIFO. Mold exposure can weaken the immune system, causing susceptibility to SIFO. For the 25% of the population that is genetically susceptible to the biotoxin illness referred to as Chronic Inflammatory Response Syndrome (CIRS), these individuals’ immune systems can’t correctly recognize mold toxins and detox them on their own. CIRS is a multi-system, multi-symptom disease caused by whole-body inflammation due to an overactive immune response triggered by biotoxin exposure such as toxic mold. This causes an even higher susceptibility to mold colonization in the gut once the individuals are in exposure. It is more likely for this specific 25% of the population to develop SIFO by breathing in mold spore fragments and particles– the mold enters the sinuses and can move through the body in mucous made within the sinuses, specifically through the post-nasal drip down the throat and into the gut. Mold fragments and particles are so small that they can also breach the blood-brain barrier (BBB).
These toxic mold particles can also find their way to the gut by landing on food and drinks. CIRS patients are at a higher risk for developing SIFO but not all will have this gut condition.
SIFO vs. SIBO
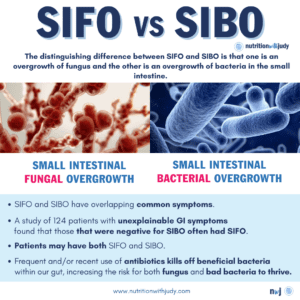
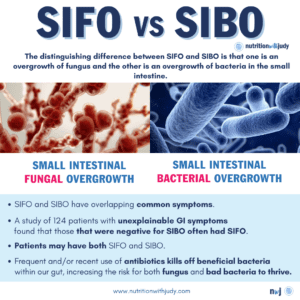
You may have heard of a condition called small intestinal bacterial overgrowth (SIBO). When it comes to symptomology, there can be a lot of overlap between SIFO and SIBO. The main difference between the two is that SIFO is a fungal overgrowth in the small intestines while SIBO is a bacterial overgrowth in the small intestines. Individuals can have both SIFO and SIBO at the same time. SIFO can occur after persistent SIBO even with proper SIBO treatment as it doesn’t target the biofilms that protect the fungal overgrowth or the fungi itself.
In one study of 124 patients with unexplainable GI symptoms, those who were negative for SIBO often had SIFO– more than 25% of the patients were diagnosed with SIFO via endoscopic testing. If you have any GI symptoms but have tested negative for SIBO, you may want to look into SIFO.
What Causes SIFO?
While the underlying mechanisms that cause SIFO are currently unclear, a 2013 study that tested 150 people for dysmotility, SIFO, and SIBO may shed some light on what causes SIFO. The study found that:
- 63% had some form of overgrowth
- 40% had SIBO
- 26% had SIFO
- 34% had both SIBO and SIFO
- 53% had dysmotility or neurological issues
- 43% used long-term proton pump inhibitors (PPIs)
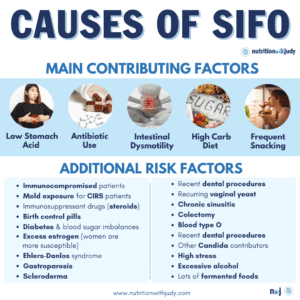
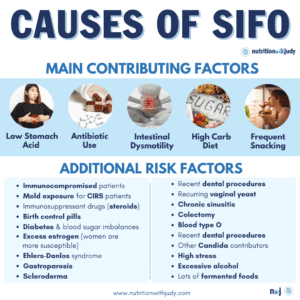
More research is needed to understand what exactly causes SIFO, but here are some of the causes that have been linked:
Low Stomach Acid and PPI Use
PPI use has been implicated as a risk factor for developing SIFO. PPIs reduce stomach acid levels, risking alterations of different bacteria and fungi strains to colonize in excess and flourish. The lack of stomach acid plays a critical role in both SIFO and SIBO– proper production of stomach acid is essential for killing fungi and bacteria before they enter the small intestines. Any over-the-counter medications that reduce acid reflux can worsen SIFO.
Some conditions can also increase the risk of low stomach acid production, such as autoimmune conditions, being over the age of 65, anemia, and the chronic use of painkillers or antacids.
Intestinal Dysmotility
We have muscles along our digestive tracts that contract, allowing substances to move through. If the contractions are slowed and less frequent, they can actually cause both constipation and diarrhea. If they’re sped up and frequent, it can cause diarrhea. This is referred to as intestinal dysmotility and is often the result of autoimmunity or disorders that cause inflammation in the intestines. Certain medications and genetic predispositions can also play a role in developing intestinal dysmotility. Patients with slow dysmotility have a higher risk of developing both SIFO and SIBO, as the muscles aren’t moving the food through efficiently. This allows food to sit in the small intestine longer, providing more opportunities for fungi and bacteria to feed and lead to over-colonization.
Recent and Frequent Use of Antibiotics
Antibiotics are notorious for significantly impacting gut health. When it comes to SIFO, the recent and frequent use of antibiotics is one of the worst causes. Antibiotics are not designed to combat fungi, viruses, or parasites. They often promote viral and fungal overgrowth because they reduce all levels of bacteria, including the beneficial strains that are supposed to help keep Candida and mold in check.
Poor Diet and Eating Habits
Any diet that’s high in sugar and carbohydrates creates the perfect feeding ground for fungal species such as yeast and molds. All sugar and carbohydrates are converted into glucose in the body, providing the optimal food for further yeast and mold colonization. Eating multiple small meals throughout the day can also be problematic for SIFO. The gut requires adequate time in order to repair while it rests, in which it rids any residual undigested material. With constant eating and snacking, the gut won’t have time to do this which creates additional food sources for both fungi and bacteria.
Other Risk Factors for Developing SIFO
In addition to PPI and antibiotics use, dysmotility, and poor eating habits, the following risk factors make individuals more susceptible to developing SIFO:
- Immunocompromised patients
- Mold exposure for CIRS patients
- Immunosuppressant drugs (steroids)
- Birth control pills
- Diabetes and imbalances in blood sugar
- Ehlers-Danlos syndrome
- Gastroparesis
- Scleroderma
- Recent dental procedures
- A high-carbohydrate diet
- Recurring vaginal yeast or chronic sinusitis
- Colectomy
- Blood type O
- Excess estrogen (women are more susceptible)
- Other Candida contributors
- High stress
- Excessive alcohol
- Lots of fermented foods
- Simple sugars and carbohydrates
What Are the Symptoms of SIFO?
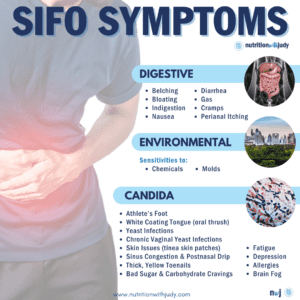
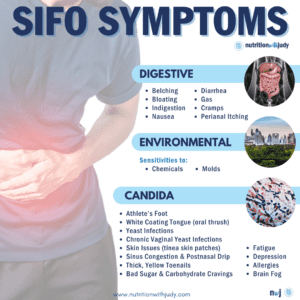
The most commonly reported symptoms of SIFO include:
- Belching
- Bloating
- Indigestion
- Nausea
- Diarrhea
- Gas
- Cramps
- Perianal itching
- Environmental sensitivities (chemicals, molds)
- Other Candida symptoms:
- White coating on the tongue (oral thrush)
- Yeast infections
- Athlete’s Foot
- Fatigue
- Depression
- Chronic vaginal yeast infections
- Allergies
- Skin issues (tinea skin patches)
- Brain fog
- Sinus congestion and postnasal drip
- Thick, yellow toenails
- Bad sugar and carbohydrate cravings
Aside from the Candida symptoms, most of these symptoms are very common which makes SIFO difficult to diagnose. It’s common for individuals with SIFO to work with multiple practitioners, take several GI tests, and still not have a proper diagnosis. A recent study discovered that fungal overgrowth in the GI tract may be the root cause for more than 25% of IBS patients– if you have IBS or have the symptoms listed above and ruled out other conditions, it may be worth looking into SIFO.
SIFO and Histamine Intolerance
Another symptom of SIFO can be histamine intolerance. Gut dysbiosis and mold are both some of the most common triggers of histamine intolerance, which can also be referred to as mast cell activation syndrome. CIRS patients with SIFO are at a higher risk of experiencing histamine issues as mast cells are triggered by the enzymes mold releases in order to break down the body’s tissues. Mold releases enzymes such as protease and hydrolyses in order to decompose the body the same way it decays a piece of food. Mast cells also react to the decomposition of tissue as a type of injury, leading to significant mast cell activation.
Pro-Tip: We don’t recommend utilizing H1 blockers long-term as these can lower the body’s production of diamine oxidase (DAO), an enzyme that helps break down histamines. H2 blockers should be avoided as these medications work by reducing stomach acid. DAO supplementation is also not ideal long-term as this acts as more of a bandaid and doesn’t address the root cause of histamine issues. Additionally, if you are taking DAO supplements long-term, make sure to test your lipase levels as we’ve seen clinically that they can increase pancreatic enzymes in a not-so-good way.
For additional histamine support, opt for herbal options while you heal.
How Do You Diagnose SIFO?
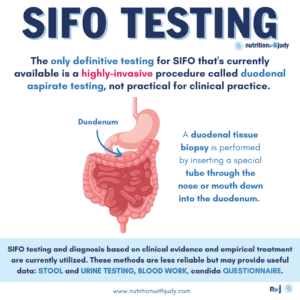
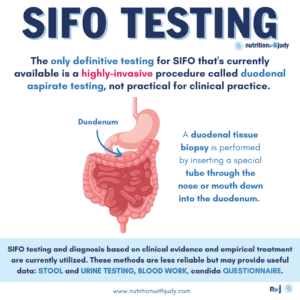
It’s important to rule out other conditions before looking into SIFO as this condition shares many overlapping symptoms with other GI infections and diseases. If your provider has worked with you to rule out other potential conditions, diagnosing SIFO can be challenging but there are different ways you can detect it. Unfortunately, the only definitive testing for SIFO that’s currently available is an invasible procedure. This procedure utilizes a small bowel or duodenal aspirate and involves removing digestive fluids from the part of the small intestine called the duodenum. The fluid sample is cultured in order to look for Candida and mold growth. Duodenal aspirate testing is a very rare, highly-invasive procedure that isn’t practical for clinical practice. Existing SIFO studies utilize this duodenal aspirate testing for research purposes only.
Certain stool and urine tests may pick up on Candida and mold overgrowth but often result in false negatives. For now, we must test and diagnose SIFO based on clinical evidence and empiric treatment. Here are the current methods available:
Blood Work
As mentioned previously, the only definitive testing method for SIFO is a highly-invasive procedure. However, there is blood work that may offer some clinical evidence for helping diagnose SIFO.
- Candida Alicans Antibodies (IgG, IgA, IgM): This antibody test isn’t always reliable. Candida can also be tested through qPCR stool tests but they won’t reveal other strains of fungal overgrowth that can result in SIFO.
- Beta-alanine: As a byproduct of Candida, beta-alanine may be elevated with SIFO.
- Secretory IgA: This marker can be tested via blood or stool. When it’s low, it can indicate SIFO. Secretory IgA is a marker of gut secretory immunity and barrier function. It’s also the main immunoglobulin found in mucous secretions and protects against potentially pathogenetic microbes due to its ability to resist degradation by enzymes and survive in harsh environments such as the GI and respiratory tracts. Secretory IgA is the first line of defense against bacteria, food residues, yeast, and parasites. Lifestyle and nutritional factors can also influence secretory IgA levels. Choline, essential fatty acids, glutathione, glycine, phosphatidylcholine, vitamin C, and zinc are all needed for efficient production.
The Candida Questionaire
The Candida Questionaire is another potential option for gathering clinical evidence for SIFO diagnosis. Not all SIFO cases are caused by Candida overgrowth so this method isn’t 100% reliable but may help with diagnostic criteria.
Each of the 11 questions below has different point totals. For every question answered “yes”, add the corresponding point value for that question. For every question answered “no”, don’t add any points.
- Have you taken prolonged or multiple courses of antibacterial/antibiotic drugs? (4 points)
- Have you experienced recurring urinary, vaginal, or prostate infections? (3 points)
- Do you feel chronically ill but haven’t discovered the root cause? (2 points)
- Are you experiencing any hormone imbalances including PMS, menstrual irregularities, sugar cravings, sexual dysfunction, fatigue, or low body temperature? (2 points)
- Are you sensitive to tobacco smoke, fragrances, and/or other chemical smells? (2 points)
- Are you experiencing any concentration or memory problems? Do you have brain fog or find yourself disassociated at times? (2 points)
- Have you taken prolonged courses of steroids and/or taken oral contraceptives for more than three years? (2 points)
- Do you have any food sensitivities or foods that trigger your GI symptoms? (1 point)
- Do you have constipation, diarrhea, bloating, and/or abdominal pain? (1 point)
- Are you experiencing any skin issues such as itching, burning, tingling, dryness, and/or rashes? (1 point)
- When you wake up in the morning, do you have a white coating on your tongue? (1 point)
Results:
- Women: You may have Candida overgrowth if your score is 10 or higher. If your score is 13 or higher, it’s very likely that Candida overgrowth is causing your symptoms.
- Men: You may have Candida overgrowth if your score is 8 or higher. If your score is 11 or higher, it’s very like that Candida overgrowth is causing your symptoms.
Other Indicators
Since it’s not uncommon for individuals to have both SIBO and SIFO, those embarking on SIBO treatment without addressing SIFO first often experience issues when trying the Elemental Diet. The Elemental Diet is 80-84% effective for eradicating all three types of SIBO: hydrogen, methane, and hydrogen sulfide. If you tried the Elemental Diet and it worsened your symptoms, SIFO could be the culprit. While the Elemental Diet can be quite effective for SIBO, it can worsen SIFO by providing some of the food sources needed for the fungal strains overgrown in the small intestinal tract.
However, individuals with histamine intolerance or dairy intolerances may not tolerate the Elemental Diet due to some of the common ingredients such as dextrose, maltodextrin, and whey protein isolate. Make sure to review ingredients before trying the Elemental Diet in order to minimize variables if you experience any symptoms. For those that have been on the carnivore diet for more than six months, have ruled out other root causes such as environmental illness, and are still experiencing GI symptoms or can’t tolerate reintroducing new foods, you may want to look into SIFO.
SIFO and CIRS
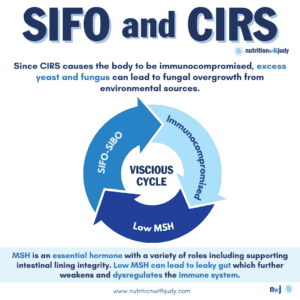
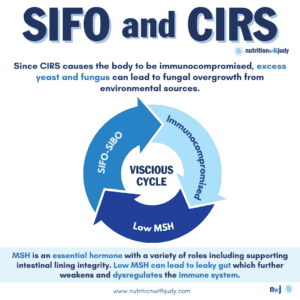
As CIRS causes the body to be immunocompromised, excess yeast and fungus can lead to fungal overgrowth from environmental sources. Since the immune system is mainly in the digestive system– 70% to 80% of the body’s immune system is in the small intestine, those suffering from CIRS often experience a vicious cycle. The gut is impaired with low melanocyte-stimulating hormone (MSH). MSH is an essential hormone with a variety of roles including supporting intestinal lining integrity– low MSH can lead to leaky gut which further weakens and deregulates the immune system. Low MSH in CIRS patients is due to the downstream effects of the biotoxin pathway along with SIFO and potentially SIBO (it’s common for CIRS patients to have both SIFO and SIBO) which further impairs the immune system. When the immune system is impaired, the gut can’t heal properly.
Removing yourself from exposure and staying in a clean environment is the first step in the Shoemaker Protocol for treating CIRS and is essential for this population that’s also dealing with SIFO. In order to achieve root-cause healing for SIFO, a clean environment combined with dietary and lifestyle recommendations and a comprehensive SIFO treatment protocol are required.
Pro-Tip: For individuals seeking comprehensive practitioner-led and community support on their mold illness journey, we welcome you to join our exclusive NwJ CIRS Group Support. Join today for access to extensive resources, a like-minded community, and unparalleled care as we journey to root-cause healing together.
SIFO and Gut Disease
As mentioned above, a recent study found that SIFO may be the root cause of over 25% of IBS patients. High levels of Candida have also been associated with the following conditions:
As more research is conducted on SIFO, it’ll be interesting to see if this could be the potential root cause for other gut conditions as well.
How Do You Prevent SIFO?


For those interested in preventing SIFO, here are our recommendations:
- Diet: A diet low in processed foods and sugars is ideal. High carbohydrate diets should also be avoided.
- Probiotics: Taking an occasional high-quality probiotic can help support proper gut function.
- Stomach acid: Make sure you have enough stomach acid production. Consider a betaine HCl supplement or digestive bitters for stimulating stomach acids. Stop the use of acid-reducing medications such as antacids and PPIs.
- Minimize certain medications: Only use antibiotics and immunosuppressants such as steroids when absolutely necessary– prioritize minimizing their use. Women should also try to avoid oral contraceptives.
- Mold exposure: Particularly for patients undergoing treatment for CIRS and those that are immunocompromised, minimizing mold exposure can help prevent fungal overgrowth from environmental sources.
How Do You Treat SIFO?
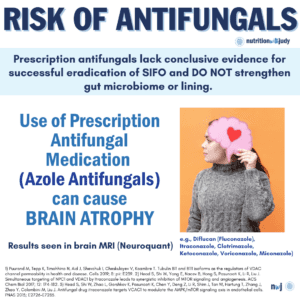
The original 2015 SIFO study recommends 2-3 weeks of antifungal therapy but continues to mention that the evidence for eradication is lacking. The concern that Dr. Shoemaker has found with prescription antifungals, particularly with the azoles class, is that they contribute to brain atrophy. We do not recommend antifungals unless all other therapies have been exhausted.
Antibiotics won’t work on SIFO since the fungal overgrowth isn’t a bacteria. Allopathic care recommends antifungal medication but this won’t resolve the root cause of SIFO. It may kill off some of the fungi but it doesn’t strengthen the gut microbiome or lining and runs the risk of brain atrophy along with other side effects.
Natural Treatments for SIFO
Dietary treatments can help rebuild the digestive system and provide bioavailable nutrients required for healing and SIFO prevention. A carnivore diet or meat-focused diet is optimal for supporting this as it offers the most bioavailable nutrition as well as gut healing support. Eating an anti-Candida diet helps starve the yeast of sugars, in turn, reducing the overgrowth of this fungal colonization. Avoiding dairy, sugar, and moldy foods can help but finding the root cause of SIFO is critical.
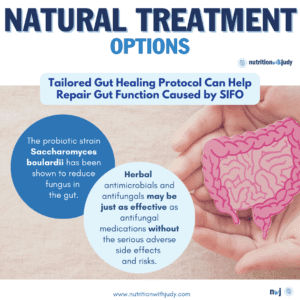
Tailored gut healing protocols, such as our Probiotic Restart Kit, can help repair impacted gut function caused by SIFO. The probiotic strain Saccharomyces boulardii has been shown to reduce fungus in the gut. RestoraFlora is a great probiotic option that contains Saccharomyces boulardii and other probiotic yeast and bacteria strains for comprehensive digestive flora support. Repairing leaky gut can also help minimize the immune system response but being able to detox or remove yeast mycotoxins, biotoxins, and other toxins is key for root-cause healing.
Herbal broad-spectrum antimicrobials and herbal antifungals may be just as effective as antifungal medications. Antimicrobials offer both antibacterial and antifungal properties, which is significant as research shows that half of patients with SIFO also have SIBO. A clinical study discovered that herbal antimicrobials were just as effective as antibiotics for treating SIBO. There currently isn’t any available research data in regards to antimicrobials for SIFO but we’ve seen success in our own clinical practice.
Our Recommended SIFO Treatment Protocol
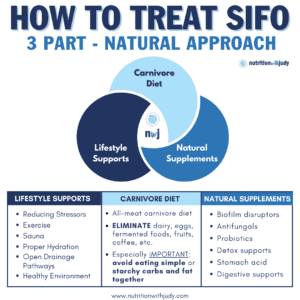
In order to properly treat SIFO, a comprehensive protocol that includes supplements, lifestyle supports, and dietary changes is required. We’ve created a foundational protocol for our clients which is further personalized based on each individual’s specific needs, detox capabilities, and medical history.
Supplements and Herbals for Treating SIFO
Working with a trusted practitioner is critical for finding the right supplement protocol for treating your SIFO. Our treatment protocol includes well-studied supports for SIFO, including biofilm disruptors for infiltrating and disrupting fungal colonies; antifungals for killing fungal overgrowth; probiotics for supporting a healthy gut microbiome and combating yeast overgrowth; detox supports for ensuring optimal detox; as well as stomach acid and digestive supports.
These are some general antimicrobials and biofilm busters that are commonly included in our SIFO protocols. It’s crucial to create a personalized protocol for you.
Lifestyle Supports
As with any treatment protocol, certain lifestyle changes can offer supplemental support while your body heals. We always recommend reducing stressors in order to allow the body to exist in a rest and digest state for optimal healing. Chronic stress causes the gut to become more permeable and the immune system to become downregulated. Finding ways to move your body, sweat, and regular sauna use are all great options for helping with additional detox, boosting mood, and supporting treatment. Additional lifestyle changes are also recommended in our SIFO treatment protocol.
The Carnivore Diet for SIFO
An all-meat carnivore diet is ideal during the SIFO treatment protocol. Eliminating dairy, eggs, fermented foods, fruits, coffee, and any other foods permitted in different variations of the carnivore diet is needed during healing. It is especially important to avoid eating simple or starchy carbs and fat together as this can worsen fungal overgrowth. If you decide to include vegetables in your diet during your SIFO protocol, it’s essential to opt for organic as both GMO and non-GMO produce are exposed to glyphosate which disrupts the gut microbiome and adversely impacts our detox pathways. There are also additional diet recommendations that are included in our SIFO treatment protocol.
After you’ve completed at least four months of our SIFO protocol, foods will need to be slowly and methodically reintroduced following the Carnivore Cure protocol. Supplements will also need to be slowly weaned off in the same way. It’s critical to work with a trusted practitioner for proper guidance on all the steps required for completing SIFO treatment.
Work With Our Trusted Carnivore Diet Functional Nutritional Therapy Practitioners
The Nutrition with Judy practice is honored to be a trusted carnivore diet practitioner support serving clients from around the globe. We’re passionate about helping our clients achieve root-cause healing in order to lead the best quality of life possible that’s nearly symptom-free. Our team is dedicated to educating our community about the incredible benefits of the carnivore diet. We welcome you to explore our free resources and are always available to support you through personalized protocols. Our Symptom Burden Assessment (SBA) is the perfect starting point for discovering your root cause and is required to work with our team— you can learn more in-depth about this powerful tool here.
Start your root-cause healing journey today and contact us any time with any questions or concerns.
DISCLAIMER: This content is for educational purposes only. While we are board-certified in holistic nutrition and are nutritional therapy practitioners, we are not providing medical advice. Whenever you start a new diet or protocol, always consult with your trusted practitioner first.




MICHAEL EDWARD ROTHMAN
August 11, 2023 at 5:59 amWow Judy! What a great presentation. Your site is amazing
Melanie
November 4, 2023 at 12:28 pmSo what happens when you’re allergic to yeast therefore can’t use s. Bouldarri? This is what happened to me. Toxic mold exposure dysregulated my immune system and not have numerous allergies, both environmental and food. One of them is yeast.
Stacy Baker
November 8, 2023 at 7:59 pmCould someone explain in more detail why eggs are on the list of foods to eliminate o the “how to treat Sifo – part 3” image?