The Carnivore Diet for Gut Health
All disease begins in the gut. – Hippocrates
With significant chronic disease and autoimmune illnesses continually on the rise, many are exploring alternative, holistic approaches to taking back their health.


With significant chronic disease and autoimmune illnesses continually on the rise, many are exploring alternative, holistic approaches to taking back their health.
Did you know that one in four Americans suffer from gut disease? Now more than ever, gut health is becoming a significant priority amongst both ill and healthy individuals. Gut health and proper digestion are two of the most important foundations for ideal overall wellness. A compromised gut can impact everything from the immune system to mental health. While there are a number of different supports and approaches required for gut healing, arguably, the most important intervention for supporting gut health is diet. Backed by considerable clinical practice, recent scientific data, and thousands of anecdotal accounts, a highly-celebrated, effective approach for optimizing gut health is the carnivore diet.
A carnivore diet is a powerful tool for addressing gut imbalances and gut disease along with all the downstream effects caused by a compromised gastrointestinal system. For some, diet intervention can promote root-cause gut healing. While for others, it offers essential support during the journey to the discovery of the foundational cause. Here is our extensive guide on the carnivore diet for gut health, the benefits it can offer, and the proper steps to take.
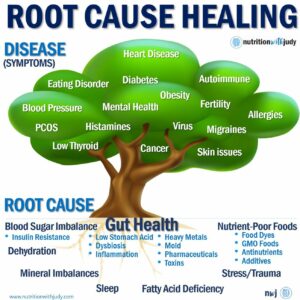
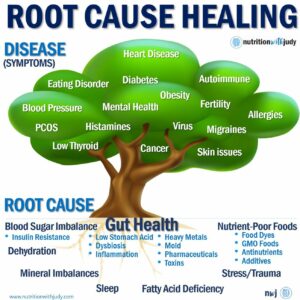
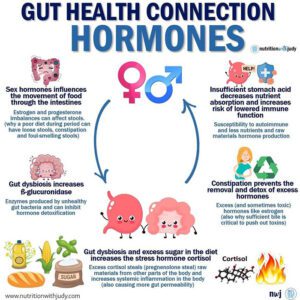
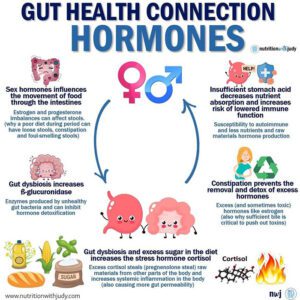
Since gut health has a direct correlation to the immune system, mental health, autoimmune disease, endocrine disorders, gastrointestinal disorders, cardiovascular disease, and cancer, we always prioritize the importance of supporting the gut in order to achieve root-cause healing. The incredible complexity of the gut and its critical role in our overall wellness is still being explored and researched.
The human microbiome, the microorganisms that live together in a specific environment, refers to the large collection of bacteria and microbes that live primarily in the gut. The body typically carries trillions of microbes in the gut, including more than a thousand species of bacteria. These bacteria not only help the body to digest foods, but they also play a critical role in immune function and mental health.
There are actually more bacterial cells in our digestive tract than there are human cells in the entire body. While there are differing opinions on the exact numbers, human cells make up only 43% of the body’s total cell count– the rest are the micro-organisms that make up the human microbiome. Research over the past 20 years has discovered that our gut flora, or microbiome, plays a critical role in regulating gut integrity and function. That’s why poor gut health including digestive issues, gut dysbiosis, and other imbalances in the gut flora can contribute to an extensive list of chronic conditions ranging from autism to rheumatoid arthritis.
So, what exactly causes poor gut health? There are a variety of factors that can impact this essential system. Since components of the gut microbiome begin to mature in utero, gut health quite literally begins in the womb. As a result of living in the modern world, gut dysbiosis and digestive problems can begin as early as birth in the following cases:
In addition to these early-stage factors, there are also other causes that can impact gut health later on. Here are the main causes of poor gut health:
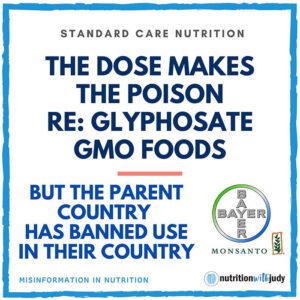
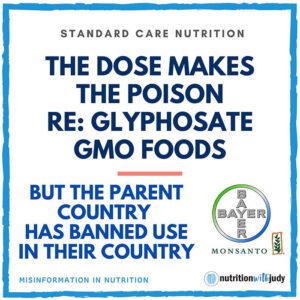
The Standard American Diet (SAD) is comprised of processed foods, highly refined carbohydrates, high sugar content, and inflammatory foods such as seed oils. All of these components impact gut health and can lead to gut dysbiosis, leaky gut syndrome, H. pylori imbalances, SIBO, and other health issues. Healthier diet variations such as paleo, Whole30, and keto can still contain foods high in plant anti-nutrients, glyphosate, and mycotoxins that can be harmful to gut health in certain individuals.
Antibiotics, oral contraceptives, NSAIDs, proton pump inhibitors (PPIs), laxatives, and other medications can all impact the gut negatively. From gut dysbiosis to leaky gut, certain medications are capable of impacting gut bacteria and impairing gut function in both short-term and long-term use. Antibiotics are one of the more prevalent culprits as they kill both good and bad bacteria. That’s why probiotic protocols are always recommended after any antibiotic use.
Individuals born with food allergies and intolerances will need to avoid specific foods in order to minimize gut damage and immune reactions. These specific foods will vary per person and why personalized elimination tools such as Nutriment are more helpful than IgG food sensitivity tests. IgG tests are not always accurate and will misrepresent sensitivities if a particular food has been removed from the diet for a while (e.g., gluten). Food intolerances differ from food sensitivities which are one of the main symptoms of leaky gut. Food sensitivities often normalize after gut healing and should ideally be reintroduced back after a successful elimination diet. Those with true food allergies and intolerances will need to avoid these triggering foods indefinitely.
Unmanaged chronic stress can wreak havoc across the body including the gastrointestinal (GI) system. Stress can impact gut bacteria and make the intestinal barrier weaker. When the brain experiences stress, it releases the stress hormones corticotropin-releasing factor (CRF), cortisol, adrenalin, and norepinephrine. Since the body can’t differentiate between chronic daily stress and life-threatening stress, it switches over to survival mode and places proper digestion on the back burner. The hormone CRF can either slow things down in the upper GI tract leading to constipation or speed things up in the lower GI tract resulting in diarrhea. Living with unmanaged chronic stress can have a significant impact on gut health.
Lifestyle considerations such as sleep, alcohol use, tobacco smoking, and drug use can all impact gut health as well. Poor sleep is another lifestyle consideration that can change the gut microbiome composition. Not only can alcohol impact the gut flora, but it is also linked to intestinal hyperpermeability, gut inflammation, and other conditions. Smoking tobacco can cause certain intestinal disorders including intestinal irritation and increased permeability of the mucosa.
Chronic GI infections from viruses, bacteria, and parasites can also compromise the gut. Infections such as salmonella, shigella, E. coli, C. diff, H. pylori, and others can all affect the digestive tract. While these infections usually result in short-term complications, certain types of infections have the potential to cause long-term consequences. Individuals that experience chronic GI infections are also more susceptible to gut imbalances and other long-term consequences.
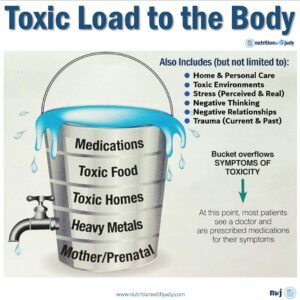
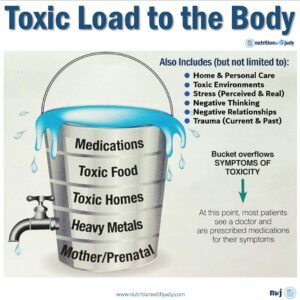
There are several studies that show how environmental toxins and chemicals can impact the gut microbiome. From heavy metals to mold mycotoxins, these toxins can disrupt the microbiome and prevent gut microbes from performing their important functions.
Some children are born with GERD-like symptoms. They have difficulties keeping breastmilk or formula down and spit up more than what should be considered normal. In these individuals, the mother’s health and family history of chronic illness should be considered. If a person has issues with gut health from a very young age, environmental toxins must be considered.


A challenge between imbalances and illness is that the symptoms can be similar and overlap. That’s why doctors and dieticians can easily misdiagnose a patient. Here are ten common signs of an unhealthy gut. The more symptoms you have, the higher the likelihood that you probably have some gut healing to do. If you’re looking for more comprehensive support in discovering if you’re suffering from a compromised gut, take our symptom burden assessment.
1. Food sensitivities: If you’re experiencing any symptoms after eating certain foods such as a histamine response or any stomach disturbances, this can signify a food sensitivity. Food sensitivities refer to IgG responses in testing but are different than a full IgE response. We don’t recommend food sensitivity testing since there is a lack of evidence supporting their findings. If you eliminate a particular type of food before the test, it will be difficult for the test to measure any sensitivities to it. While many people develop food sensitivities and have an immune response due to compromised gut health, there are certain people that are born with food allergies (IgE reaction) and intolerances to food such as nuts.
2. Bloating after every meal: While bloating might be common, it isn’t normal, especially after every meal. Bloating after every meal may be a sign of chronic indigestion or dyspepsia. If you experience bloating as soon as you eat, this may be more upper GI-related, for instance, an issue with the stomach. If you experience bloating an hour or two after you eat, this may be related to issues in the small or large intestine.
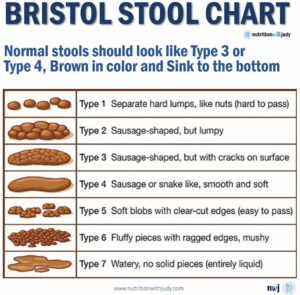
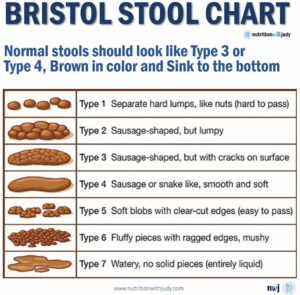
3. Inconsistent stools and excess gas: If your bowel movements aren’t consistent with brown, solid stools that sink to the bottom of the toilet, you have inconsistent stools. Experiencing loose stools one day and constipation the next can also be a signifier of an unhealthy gut. Excess gas can be related to underlying digestive health issues such as indigestion or IBS.
4. Feeling better when not eating: If eating causes cramping, abdominal pain, or any other discomfort, you may need some gut healing. However, if you experience worse energy after a meal, this may be a blood sugar imbalance issue. Blood sugar imbalance can have a role in exacerbating an imbalanced gut but generally speaking, the symptomology that’s pertinent for this is related more to physical pain after eating.
5. Skin imbalances: The skin microbiome has just as many trillions of bacteria, fungi, viruses, and small microbes as the gut. Referred to as the gut-skin axis, the gut and skin biomes have a bidirectional relationship and are both responsible for critical immune and neuro-endocrine roles. They’re also both uniquely related in purpose and function. If you struggle with acne, eczema, psoriasis, and other skin flares, you probably need gut healing support. Skin imbalances may also signify impacted gut function such as poor nutrient absorption.


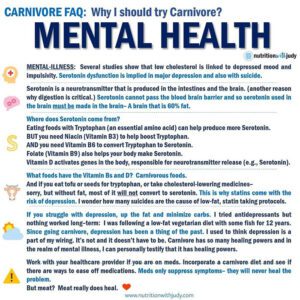
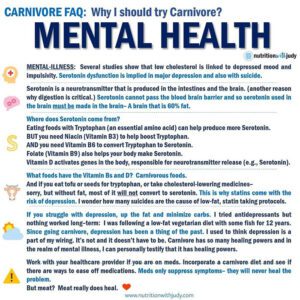
6. Sleep disturbances: There can be a variety of driving factors that cause long-term sleep disturbances. If you’ve ruled out blood sugar imbalances and struggle to sleep through the night on most days, you may have an unhealthy gut or a deeper root cause issue such as CIRS. Proper sleep is needed for the balance of leptin and ghrelin, two very important hormones that regulate hunger and satiety. One study reported that just one night of sleep deprivation can increase ghrelin levels, the hunger cue hormone, and feelings of hunger in healthy, normal-weight men. Another reason our gut can disturb our sleep is due to the fact that approximately 95% of our total body’s serotonin is produced in our gut. Serotonin is a neurotransmitter that helps balance mood, cognition, learning, memory, and many other processes. Sufficient serotonin levels are required for producing melatonin, the hormone responsible for regulating sleep. With gut imbalances, we won’t produce enough serotonin or melatonin, which is another reason why mental health is always impacted by our gut health.
7. Chronic fatigue and imbalanced adrenal sufficiency: One of the essential functions of the gut is to absorb nutrients for energy. If gut function is impaired and incapable of proper nutrient absorption on top of being chronically inflamed from gut imbalances, low doses of cortisol will be pushed out in order to support the gut. Eventually, this can lead to constant fatigue and poor endocrine health (the system your adrenals are a part of). Constant fatigue can be a sign of small intestinal bacteria overgrowth (SIBO). Having more harmful gut bugs than good creates imbalances that can cause symptoms of chronic fatigue and imbalanced adrenal sufficiency.
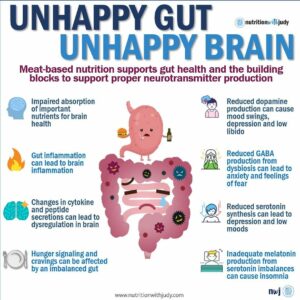
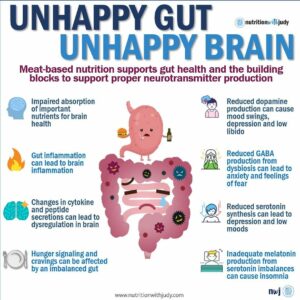
8. Mental health imbalances: The gut-brain axis explores the influence of gut microbiota on the central nervous system and mood. Imbalances in the gut flora can directly impact your mood. Mental health can also suffer from impaired gut function due to a lack of nutrient absorption required for creating neurotransmitters. Experiencing chronic gut issues can also exacerbate mental health imbalances. Additionally, consistent gut pain or feeling chronically ill can impact overall mood and mental health.
9. Weakened immune system: Approximately 70% to 80% of the immune system is in the small intestine. If the small intestine experiences damage resulting in holes and gaps (this condition is called leaky gut syndrome), this creates the inability to absorb nutrients and fight off invaders. These small food particles and possible toxins find their way to our bloodstream and lead to a higher risk of autoimmune illness and additional food sensitivities.
10. Low stomach acid: Stomach acid is responsible for breaking down food, absorbing nutrients, and defending against pathogens. Low stomach acid can be caused by vitamin deficiency, stress, medications, alcohol consumption, older age, and other factors. Having low stomach acid leads to impaired digestion, increased susceptibility to infection, and reduced nutrient absorption. Symptoms present as bloating, burping, upset stomach, heartburn, diarrhea, GI infections, undigested food in stool, gas, and more.
Just like most chronic conditions, gut disease may not be the root cause. We’ve encountered many patients that have a gut disease diagnosis from a practitioner and simply accept that there’s no treatment and that they have to be on life-long medication for symptom management. In a study conducted by the Mayo Clinic, they found that up to 88% of second opinions or diagnosis confirmations differ from the first diagnosis (e.g., gut disease and autoimmunity). Not only are there flaws in confirming a diagnosis, but in most cases, these gut conditions are treatable. Once a person cleans up their diet, eats mostly carnivore-based, and follows a temporary gut support protocol, gut issues should improve. If the gut imbalances don’t subside, gut disease may be a symptom of a bigger root cause imbalance. Once you find the root cause and start a healing protocol, your gut disease should subside as well.
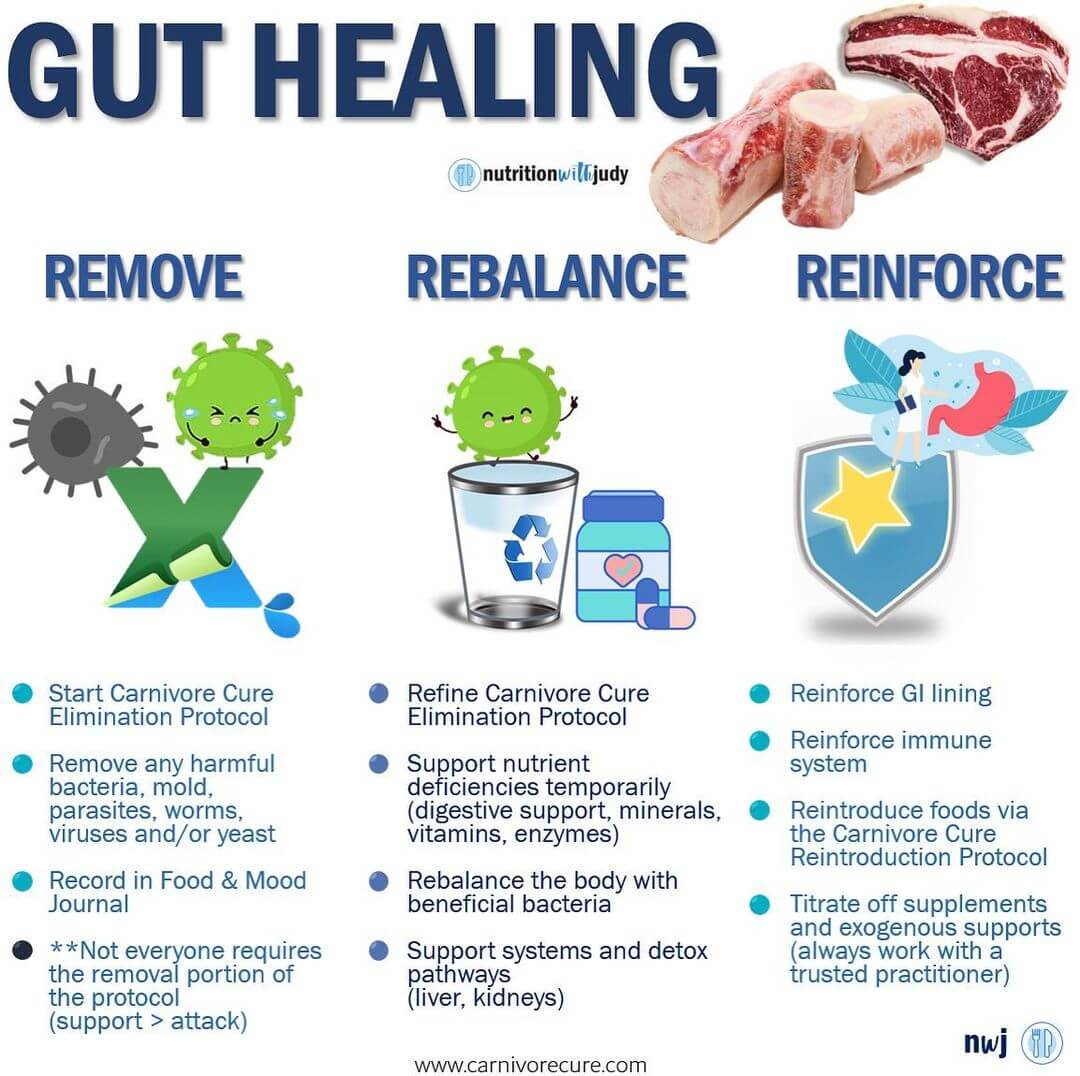
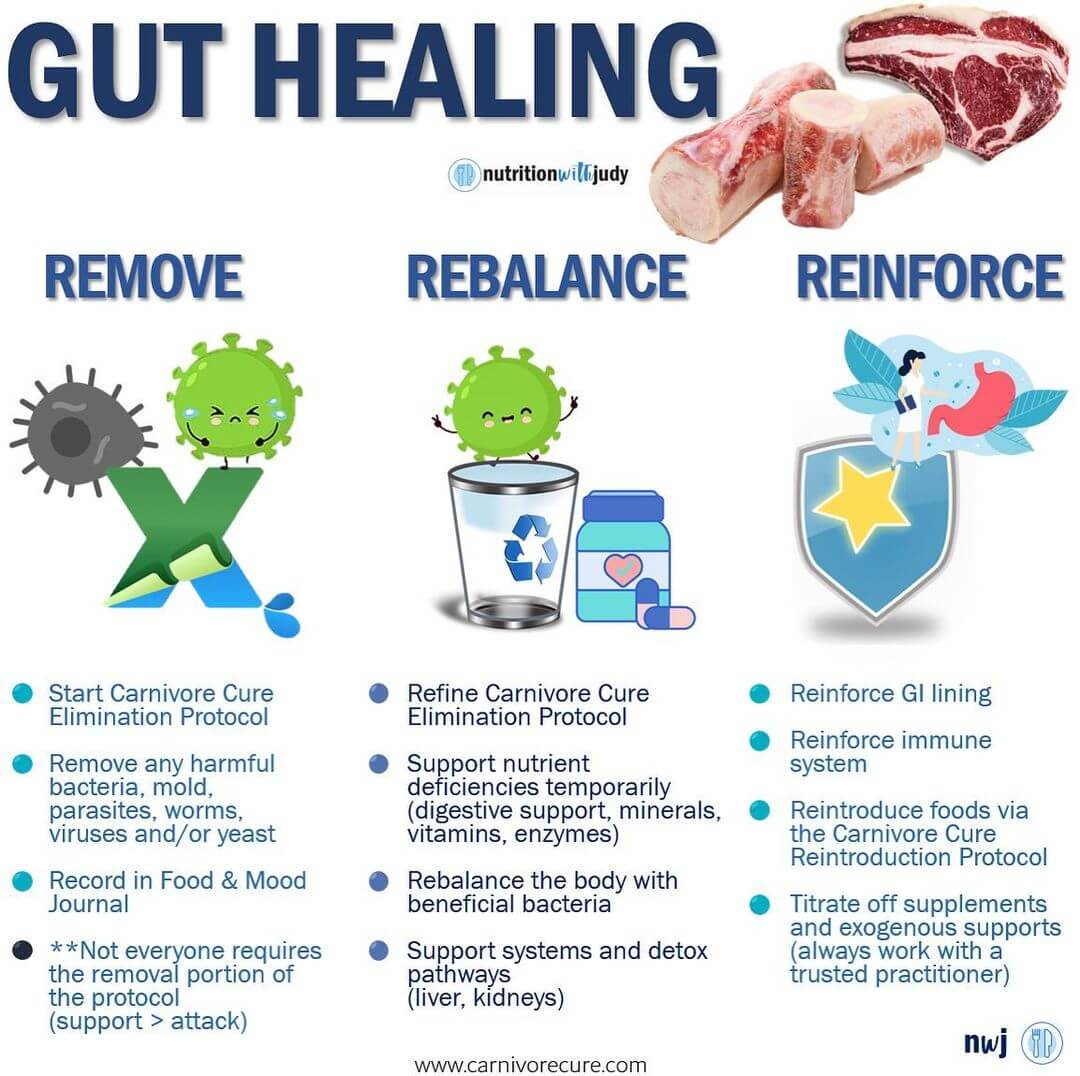
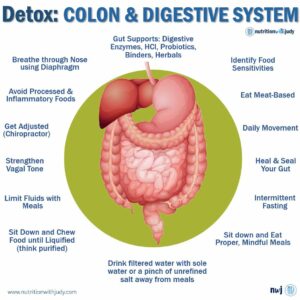
Now that we have a better understanding of how important gut health is, its role in chronic illness, and what compromises the gut, how exactly do you heal it? A gut healing protocol requires a comprehensive, personalized approach since there are so many different factors that are at play here. Generally speaking, here are the foundational steps required for gut healing:
In certain cases that involve worms, parasites, and mold, you won’t achieve root-cause healing until you remove these toxins. If you have significant gut issues, you may want to work with a practitioner to do some initial tests to rule out these culprits. Not everyone will require this, however, implementing the Carnivore Cure Elimination Protocol which utilizes a carnivore diet is key. This allows you to remove all potentially problematic foods.
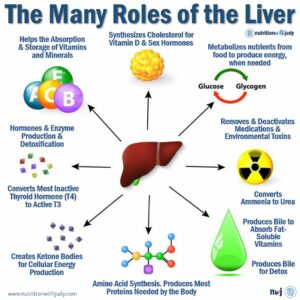
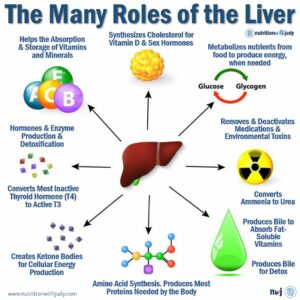
During the rebalance stage, it’s ideal to refine the Carnivore Cure Elimination Protocol and focus on rebalancing the body. Rebalancing the body’s beneficial bacteria and supporting nutrient deficiencies temporarily as the gut heals are important bandaids. While removing toxic pathogens, most practitioners will use nutritional support to help the detox pathways such as the liver and kidneys. Supports such as digestive enzymes, minerals, vitamins, and probiotics are also used short-term to help impaired gut function until healing is achieved and these are no longer needed.
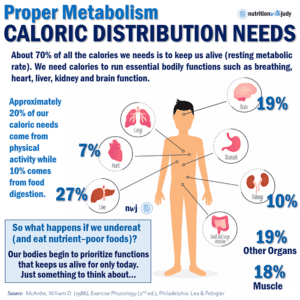
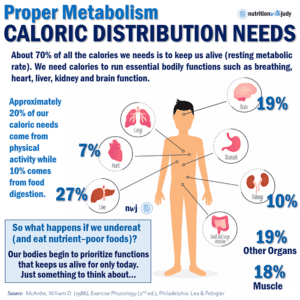
The last step is reinforcing the GI lining and immune system. Since 70% to 80% of the body’s immune system is in the small intestine, this is essential for both a healthy gut and overall wellness. Reintroduction of foods through the Carnivore Cure Reintroduction Protocol can also take place, helping individuals fine-tune their diet for long-term sustainability and personalized needs. As impaired gut function subsides, individuals can also titrate off of supplements and exogenous supports. We always recommend working with your trusted practitioner for this.
The Carnivore Cure is the first elimination protocol that explains how to adopt a carnivore diet for healing purposes. It’s an essential step for starting any gut healing protocol so you can find root-cause healing. You can read more about how to implement this elimination diet protocol here.
The first step is implementing the right elimination diet for supporting the gut and helping it heal. There are other supports that we’ll discuss after delving into the carnivore diet for gut health.
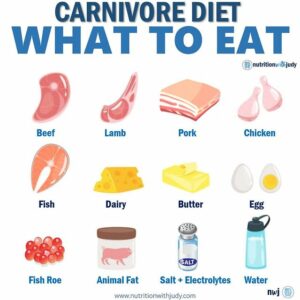
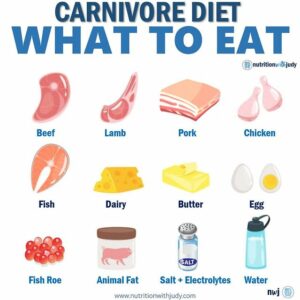
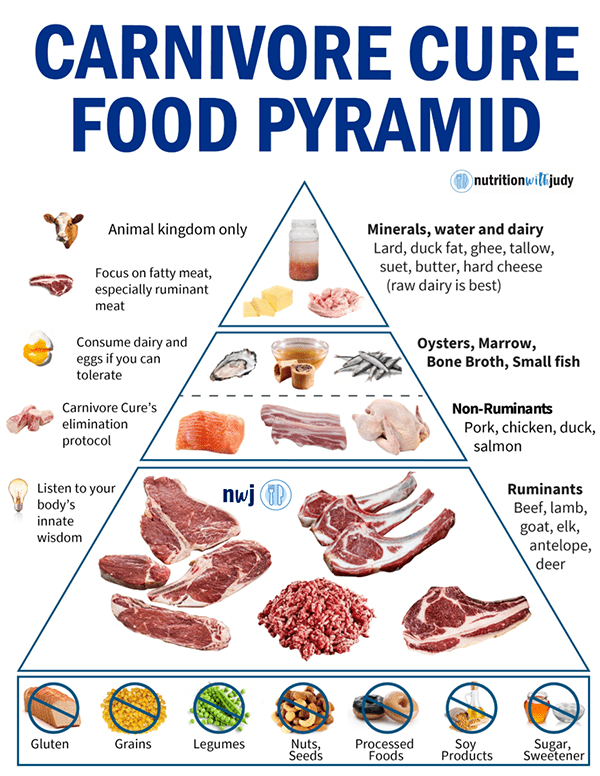
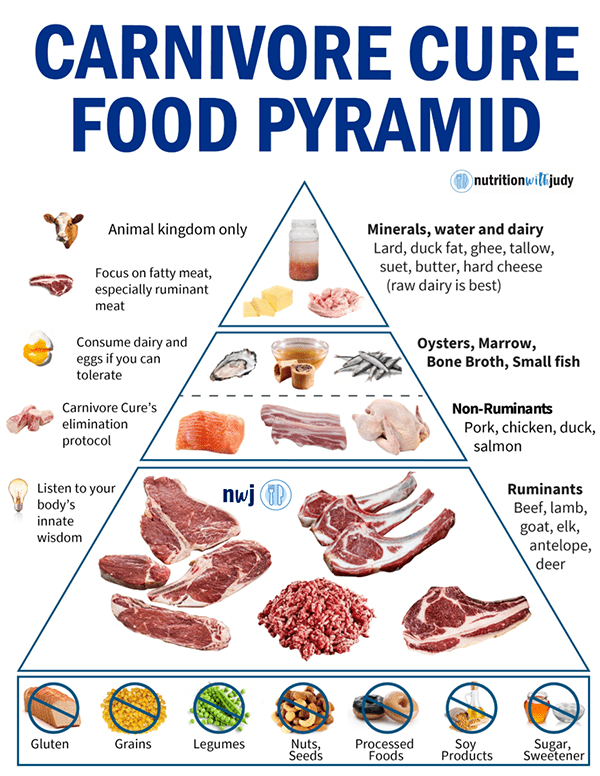
The carnivore diet consists of eating only animals and avoiding all plants and grains. It is a true zero-carb or nearly zero-carb way of eating that focuses solely on animal proteins and fats. There are many variations of this diet that are defined by various restrictions and inclusions of certain foods. However, not all are recommended especially when it comes to gut health. A more intentional elimination approach is ideal for those interested in utilizing this diet for healing the gut. Learn more about the basics of the carnivore diet here.
All elimination diets provide some relief since they eliminate important culprits such as processed foods, refined foods, and particularly inflammatory seed and vegetable oils. However, when you have gut dysbiosis, an imbalance of excess bad gut bugs, food sensitivities don’t disappear by merely removing the guilty food groups. The most significant pitfall of all elimination diets is that they focus on which foods to remove and retain depending on the person’s sensitivities, but these diets rarely prioritize essential nutrients.
Several elimination diets show that it’s possible to use them to start healing and attaining optimal health. However, it’s clear that no single diet or protocol works for everyone. Most of the popular elimination diets such as the autoimmune paleo diet (AIP), FODMAP, GAPS, Whole30, and low histamine diet, are great ways to find the foods you should eat to minimize symptoms. But all these protocols have one thing in common: they include most fruits and vegetables. But what if one of the real culprits is plant-based foods? That’s why a carnivore diet elimination approach begins with only the most fundamental foods and is more restrictive to rule out potentially problematic plant foods. A carnivore diet also helps maximize healing by providing the body with the most bioavailable nutrient-dense foods.
The carnivore diet is celebrated for its many benefits ranging from lower inflammation to mental clarity. Utilizing this tool for gut healing is optimal as this helps us discover root-cause healing. In addition to being the ultimate elimination diet, the carnivore diet is ideal for supporting gut health for a number of reasons:
The duration of the carnivore diet needed for gut healing is very patient-dependent. Some individuals will only need a month before they’re able to reintroduce foods from the plant kingdom while others with severely impaired gut function and potential additional root causes may require several months or more. Working with a trusted practitioner can help guide you through this process.
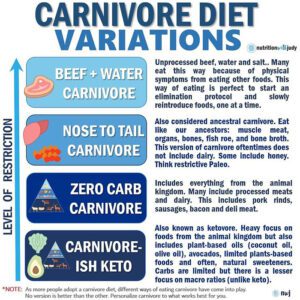
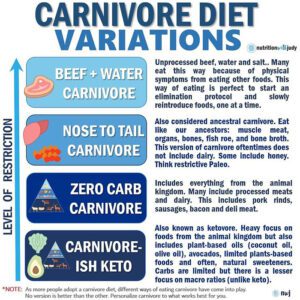
There are different variations of the carnivore diet you can explore. However, for the purpose of gut healing, we recommend taking a more restrictive approach, to begin with. This is especially true if you have a gut disease, a compromised gut, autoimmunity, or other chronic conditions. It’s ideal to start with beef-only carnivore or the Lion Diet (ruminant animals, salt, and water only) before expanding into other animal kingdom foods and then eventually reintroducing plant foods. Starting as clean as possible allows you to really determine food sensitivities so you can avoid these while you heal.
Consider including the following foods for gut healing, if tolerated:


It’s ideal to start with the highest-quality meats that are accessible to you. This isn’t always required as many people can experience gut healing from conventional grain-fed meats. The most important thing is focusing on animal kingdom foods and purchasing what you can afford. However, individuals with autoimmune conditions, histamine intolerance, and significant gut damage may need to focus on sourcing higher-quality meats, to begin with. Think ruminant animals that are grass-finished and unaged, pork and poultry that’s pastured and corn/soy free, wild-caught seafood, and pastured corn/soy-free eggs.
The carnivore diet will require some special considerations if you have histamine intolerance. Depending on how sensitive you are, sourcing the freshest meat possible whether from your local butcher or purchasing from a specialty unaged farm online will be ideal. Certain carnivore foods including shellfish, fish roe, some dairy products, and bone broth have higher histamine content and should be avoided while healing. Egg yolks have low histamine content while the whites are high histamine, so you may want to experiment with yolks only, but some individuals will need to avoid eggs completely. Duck and quail eggs are also options that seem to be tolerated better by sensitive individuals.
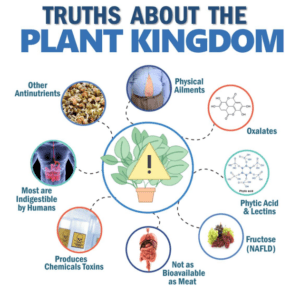
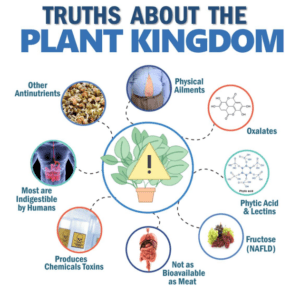
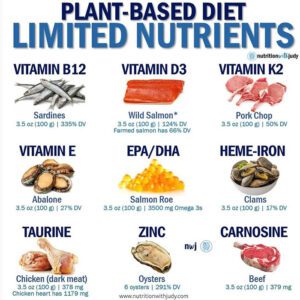
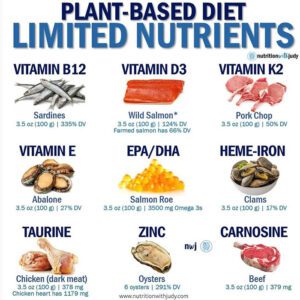
While certain plant foods may contain some of the same nutrients found in meat, there are many issues at hand here. Bioavailability is key and many of the nutrients and antioxidants promoted in plants aren’t actually being absorbed by the body. Studies show that plant protein is far less digestible and bioavailable, and has a less favorable amino acid profile when compared to animal protein. Anti-nutrients such as phytic acid, which is naturally occurring in seeds, legumes, nuts, grains, and more, inhibit the absorption of minerals. There are also essential nutrients that are only found in animal foods, causing nutritional deficiencies if eating plant-based.
Additionally, the plant kingdom is filled with other anti-nutrients such as lectins and oxalates, often have glyphosate herbicide exposure, and can also be contaminated with mycotoxins due to farming and storage practices. Lectins and many other anti-nutrients are infamous for causing further gut permeability, meaning holes in the mucosal lining.
The animal kingdom is rich in bioavailable nutrients that are essential for optimizing gut health in addition to overall wellness:
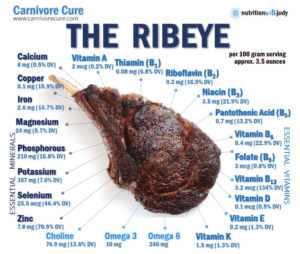
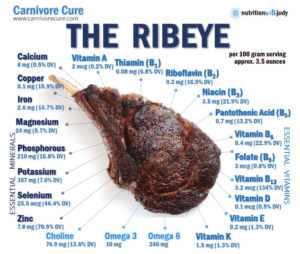
The ribeye is one of the most beloved cuts in the carnivore diet and for very good reason. A ribeye steak has nearly all the essential minerals and vitamins for overall wellness and supporting gut health. It also contains a good amount of omega-3 and omega-6 fatty acids in addition to choline, creatine, and carnosine.
Note: Not all nutrient deficiencies are the underlying root-cause issue. Sometimes it’s not a food issue but a metabolic or gut imbalance that causes nutritional imbalances to manifest. Don’t play mad chemist with supplements.
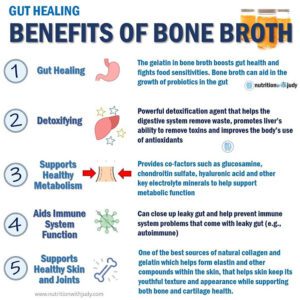
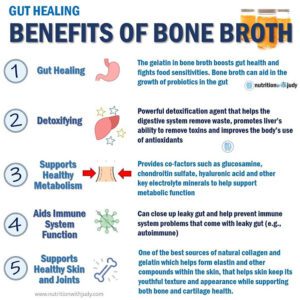
Bone broth is one of the most nutrient-dense foods and offers benefits for every single part of the body. It’s renowned for its collagen and gelatin content which are key for digestive and gut health among others. Bone broth also contains glycosaminoglycans that support elastin and collagen, and are critical for the colonization and proliferation of gut bacteria. High-quality bone broths should contain 19 essential and non-essential amino acids, eight of the 13 essential vitamins, and 15 of the 20 essential minerals (16 if you add iodine from fish bones).
Bone broth supports gut healing and may even be better than fatty cuts of meat. Our digestive system needs to properly break down meats into amino acids and fatty acids for nutrient absorption. Easily digestible proteins such as bone broth can support gut healing while a leaky gut can take longer to heal with too much protein (digestive aids and removing stress can also help).
It’s important to note that if you have histamine intolerance or responses, you may need to avoid bone broth as you heal. You can reduce some of the histamine response by cooking frozen or fresh unaged bones in a pressure cooker for less time and freezing it in an ice cube tray for smaller portions. That’s one of the reasons why homemade bone broth is ideal. As your gut heals, you should be able to tolerate bone broth without a histamine response. Meat broth cooked with only low-histamine meat, salt, and water is a great lower-histamine option for those that don’t tolerate bone broth.
We always advocate for eating a variety from the animal kingdom if possible. You may not be able to eat specific meats, dairy products, or bone broth to begin with, but as you heal, the gut should start tolerating more and more. Here are some powerful gut-healing nutrients found in other carnivore foods outside of beef and bone broth:
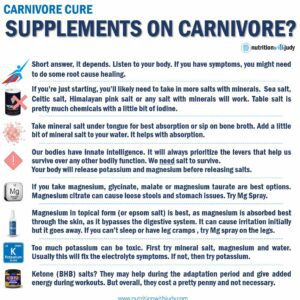
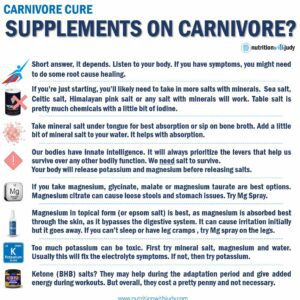
Generally, most people transitioning to a carnivore diet will only need to focus on electrolytes and temporary supports as their gut adjusts to producing more stomach acid and sluggish gallbladders catch up to new higher fat intakes.
In our clinical practice, those with severely impaired gut function will require additional gut support in addition to the carnivore diet for optimal gut healing. When starting the carnivore diet, these patients often find that general digestive symptoms improve but not fully. If you’re still teetering between loose stools and constipation weekly, get nauseous with too much fat, or have indigestion or gas after a carnivore meal, you probably need some gut support.
If your digestive process isn’t functioning at capacity, it won’t be able to break down your foods into the raw materials it needs to fuel and heal the body, including the gut. It doesn’t matter how great your food quality is if you are not properly absorbing your nutrients.
We always recommend working with a trusted practitioner before starting any new supplement protocols or diets– if you’re still experiencing gut symptoms on the carnivore diet and are interested in comprehensive support for your gut healing journey, check out our 3-Month Wellness Package with Symptom Burden Assessment.
Here are some temporary supports that we use with our clients. These are general supports that focus on healing locally (e.g., stomach, liver, and/or small intestine) but until we find the root cause, it’s not an exact science. No specific supplement works for everyone but these are some of our go-to’s for our carnivore clients:
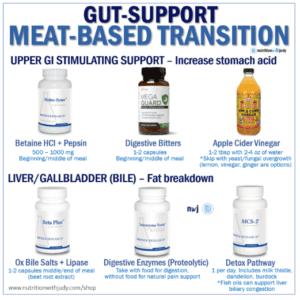
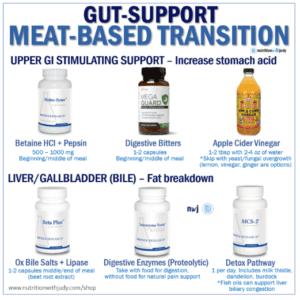
Betaine Hydrochloric Acid (HCl) is very effective for low stomach acid, GERD, and indigestion. However, HCI shouldn’t be taken if you’re using any type of anti-inflammatory medication such as corticosteroids, ibuprofen, or NSAIDs on a daily basis. When taken together, it can damage the GI lining. Almost 90% of Americans are deficient in hydrochloric acid. HCl supplements help to provide additional digestive support and hydrochloric acid for improved absorption of nutrients. Hydro-Zyme supports the gut with supplemental hydrochloride, pepsin, pancreatin, and other known synergists. Betaine Plus HP has a greater amount of betaine HCl and pepsin if you need stronger support.
Digestive enzymes also work well for additional support. We’ve slammed our pancreas with excess insulin production and now can’t produce enough digestive enzymes to break down our foods, particularly fats and proteins. There are different types of digestive enzymes including proteolytic enzymes. Intenzyme Forte contains proteolytic enzymes that mimic the ones in your body and are tolerated by most. In case you’re concerned, taking more digestive enzymes or HCl won’t shut down your body’s natural production of them. For individuals with histamine concerns, you may not tolerate proteolytic enzymes. Bio-6-Plus is another great digestive enzyme to explore if you have histamine concerns.
Fish oils are another avenue to explore if you’re still experiencing loose stools. Fish oils such as gut-specific MegaOmega may help with overall liver support so you can better produce bile for fat breakdown and toxin removal. However, those with histamine intolerance generally do not tolerate fish oil supplements. OMAPREM SPM Resolvins are another beneficial fatty acid supplement to explore. Clinical studies show its efficacy in reducing severe chronic pain for a variety of conditions including osteoarthritis, rheumatoid disorders, and athletic performance soreness. SPM Resolvins can also be utilized to lower MMP-9 in CIRS, which is an inflammatory marker.
High-dose vitamins such as choline and riboflavin are other options you can try to help resolve loose stools. Make sure to work with your trusted practitioner in order to determine if this option is safe for you and your gut healing journey.
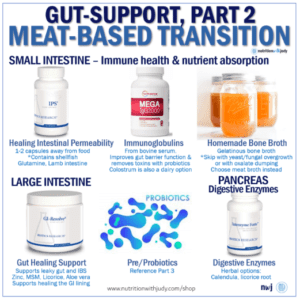
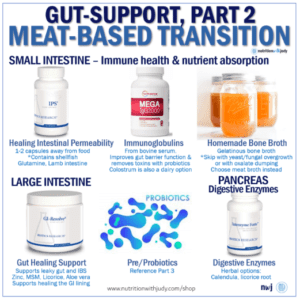
Small intestine herbals such as IPS can help promote small intestinal healing. Since the small intestine houses most of the body’s immune cells and is also where most of our nutrients are absorbed, it’s critical for gut health. IPS does contain shellfish so not everyone can take it.
Immunoglobulins (IgGs) are a great option for helping improve immune function. Since not everyone can tolerate dairy, we often recommend an IgG supplement called MegaIgG2000 instead of colostrum. If you do tolerate dairy, colostrum can be another option to explore for immune function.
General eradicating supports such as herbal antifungals may be needed for things such as SIBO and SIFO. However, we believe in healing the body first before attacking it. One way we support the body with less proliferation of toxins is by sticking to a cleaner diet, such as the carnivore diet, while we strengthen the body. Other supports include oregano oil (which doesn’t usually help with strong imbalances), caprylic acid (MCT oil, C8), MSM, Saccharomyces boulardii, dill, and garlic may be used for SIBO eradication. Note: It’s especially important to work with a practitioner when treating SIBO and SIFO.
Herbals such as marshmallow root, slippery elm, and licorice root can help support both the large and small intestines. GI Resolve contains all three in addition to other herbals for promoting optimal function of the GI lining, rejuvenating intestinal mucosa, and building immune support.
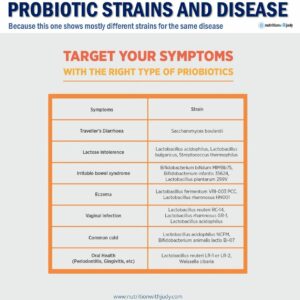
An important note about probiotics– no one really knows what strains are the best for us. We’ve mapped the human genome, studied populations of people’s healthy and sick guts, and preliminarily decided which strains are likely good for us. However, we don’t have any conclusive evidence. This is especially true for someone who eats a carnivore diet. But generally speaking, there are basic umbrella probiotics that have shown efficacy for gut health in our practice.
Another thing to note is that probiotics don’t live and survive in the body, they only work while taking them. That means that these should be used as temporary supports during healing and why focusing on a clean diet long-term is so important. The only probiotic that can live and proliferate in the body is spore (soil-based) probiotics.
These are the major umbrella probiotics that essentially cover the majority of the strains available:
*Note: Half of our clients don’t do well with this product since it includes prebiotics and has strains that may elicit a histamine response. Try a different product that contains these probiotic strains but without the prebiotic fibers. Those with histamine intolerance will need to find low-histamine probiotic strains.
If you’ve taken antibiotics or had traveler’s food poisoning, you may want to try our full Probiotic Restart Kit. It’s a very powerful probiotic kit that has helped many of our clients. These probiotics are also safe for infants and children but make sure to start with smaller doses.
If you’re concerned with plant anti-nutrients, most supplements (unless it’s an extract) will have most of these compounds removed. Remember, these are meant to be only temporary supports as you heal. If you’re unable to successfully titrate off of these without experiencing symptoms after long-term use, you’ll need to find the root cause.
We always recommend trying one at a time and moving up slowly to the proper dose. You don’t want to overwhelm the system and you also want to rule out what’s helping and what’s not. As a reminder, these are general supports and won’t necessarily work for you. It may take some fine-tuning to discover what supports are helpful based on your specific sensitivities and individual needs.
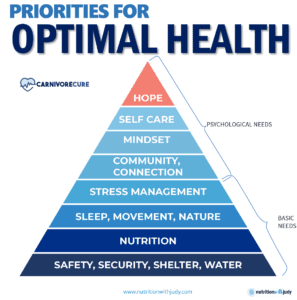
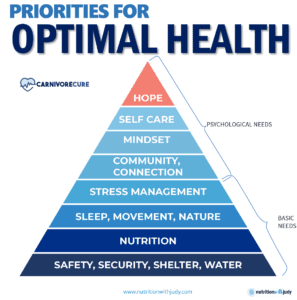
In addition to the carnivore diet and temporary gut healing supplements that help rebalance the microbiome and enhance nutrient absorption, there are other significant things you can implement to help support your gut health. Genetics can absolutely play a role in gut health but as the study of epigenetics believes, our lifestyle determines what genes are turned on and off. Eating a carnivore diet can do wonders for our gut but the following supports can be just as important:
Reducing stress is critical to gut health. If you have chronic stress in the body, it creates chronic, low-dose inflammation. This can include mental stressors, trauma, and even physical stress. Chronic stress is toxic– it weakens the immune system, causes more gut permeability, and causes the endocrine system to prioritize using raw materials to produce high levels of cortisol. Unmanaged stress can also reshape the gut bacteria’s composition through stress hormones, inflammation, and autonomic alterations. This causes gut bacteria to release metabolites, toxins, and neurohormones that can also alter eating behavior and mood.
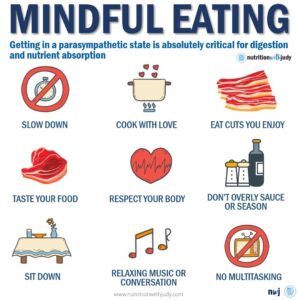
It can be tricky pinpointing if your sleep habits are exacerbating gut issues, if your compromised gut is responsible for impacting your sleep, or a bit of both. Regardless, prioritizing quality, consistent sleep is key for gut healing as well as overall wellness. Insufficient sleep can influence how much you eat and preliminary research is showing that sleep is also linked to the way the gut functions. There are also studies that suggest that a lack of sleep may be linked to a reduction of healthy microbes in the gut. When you don’t get quality sleep, your cortisol is higher in the morning which causes a reduction in immune and digestive function, which often can, symptomology-wise, be seen as cravings the next day. Some healthy eating habits to implement for better sleep include: finishing eating at least two to three hours ideally before bed, practicing mindful eating by chewing your food thoroughly and slowly, reducing or eliminating caffeine and alcohol intake, and exploring better sleep positions that reduce GI symptoms including sleeping on your left side and/or propping your head up.
Did you know that exercise and movement have as much power as taking an antidepressant? Not only is it incredible for mental health and overall wellness, but it also is essential for gut healing. Many studies support that moderate endurance exercise reduces inflammation and improves body composition, leading to positive effects on gut microbial diversity by enhancing the number of beneficial microbial species. It also has the capability of strengthening the muscles in the gastrointestinal tract for enhancing intestinal contractions. In turn, exercise may ease constipation and improve the frequency of bowel movements. Exercise also strengthens the immune system, boosts mucosal immunity in the gut, improves your metabolism, and helps reduce stress.
The Nutrition with Judy practice is honored to be a trusted carnivore diet practitioner support serving clients from around the globe. We’re passionate about helping our clients achieve root-cause healing in order to lead the best quality of life possible that’s nearly symptom-free. Our team is dedicated to educating our community about the incredible benefits of the carnivore diet. We welcome you to read our extensive free gut healing resources and are always available if you’re looking for personalized support. Our Symptom Burden Assessment (SBA) is the perfect starting point for discovering your root cause and is required to work with our team— you can learn more in-depth about this powerful tool here.
Start your root-cause healing journey today and contact us any time with any questions or concerns.
DISCLAIMER: This content is for educational purposes only. While we are board-certified in holistic nutrition and are nutritional therapy practitioners, we are not providing medical advice. Whenever you start a new diet or protocol, always consult with your trusted practitioner first.