Does Red Meat Help With Anemia?
Nutritional deficiencies can wreak havoc across the body and can sometimes even be the root cause of certain symptoms and conditions. Did you know that iron deficiency, also known as iron-deficiency anemia (IDA), is the number one nutritional deficiency across the globe? IDA is the most common type of anemia. IDA affects nearly 2 billion people a year with young children and women accounting for the largest percentage of cases. IDA also affects 33% of the global population and isn’t just a problem in developing countries—4 to 5 million Americans suffer annually.
A common question we receive regarding anemia is, does red meat help with anemia? Let’s take a closer look at what causes anemia, the importance of iron, and the best ways to treat IDA.
What Is Anemia?
Anemia is a condition where the body doesn’t have enough healthy red blood cells or hemoglobin in order to carry oxygen to the body’s tissues. Hemoglobin is a type of protein in red blood cells that carries oxygen from the lungs to all of the other organs in the body. There are many forms of anemia with various causes and severities that can present both short-term and long-term.
Types of Anemia
While this article covers iron-deficiency anemia, here are the other types of anemia:
- Aplastic anemia: This rare form of anemia is a condition that happens when the body stops producing enough new blood cells. Individuals with aplastic anemia often feel fatigued and can be more prone to uncontrolled bleeding and infections. Treatment may include prescription medications, blood infusions, or stem cell/bone marrow transplants.
- Sickle cell anemia: Sickle cell anemia is an inherited disorder that affects the shape of red blood cells. Red blood cells are generally round and flexible, but with this disorder, the blood cells become shaped like sickles or crescent moons. There’s no cure– treatments include pain relief and complication prevention.
- Thalassemia: This type of anemia is another inherited blood disorder that causes the body to have less hemoglobin than required. Mild thalassemia may not require any treatment, but more severe cases may require regular blood infusions.
- Vitamin deficiency anemia: Vitamin deficiency anemia is characterized as a lack of healthy red blood cells, which is caused by deficiencies in vitamin B12 and folate. Individuals not consuming enough foods rich in B12 and folate as well as those with methylation and nutrient absorption problems, are at risk of developing this form of anemia.
Iron-Deficiency Anemia
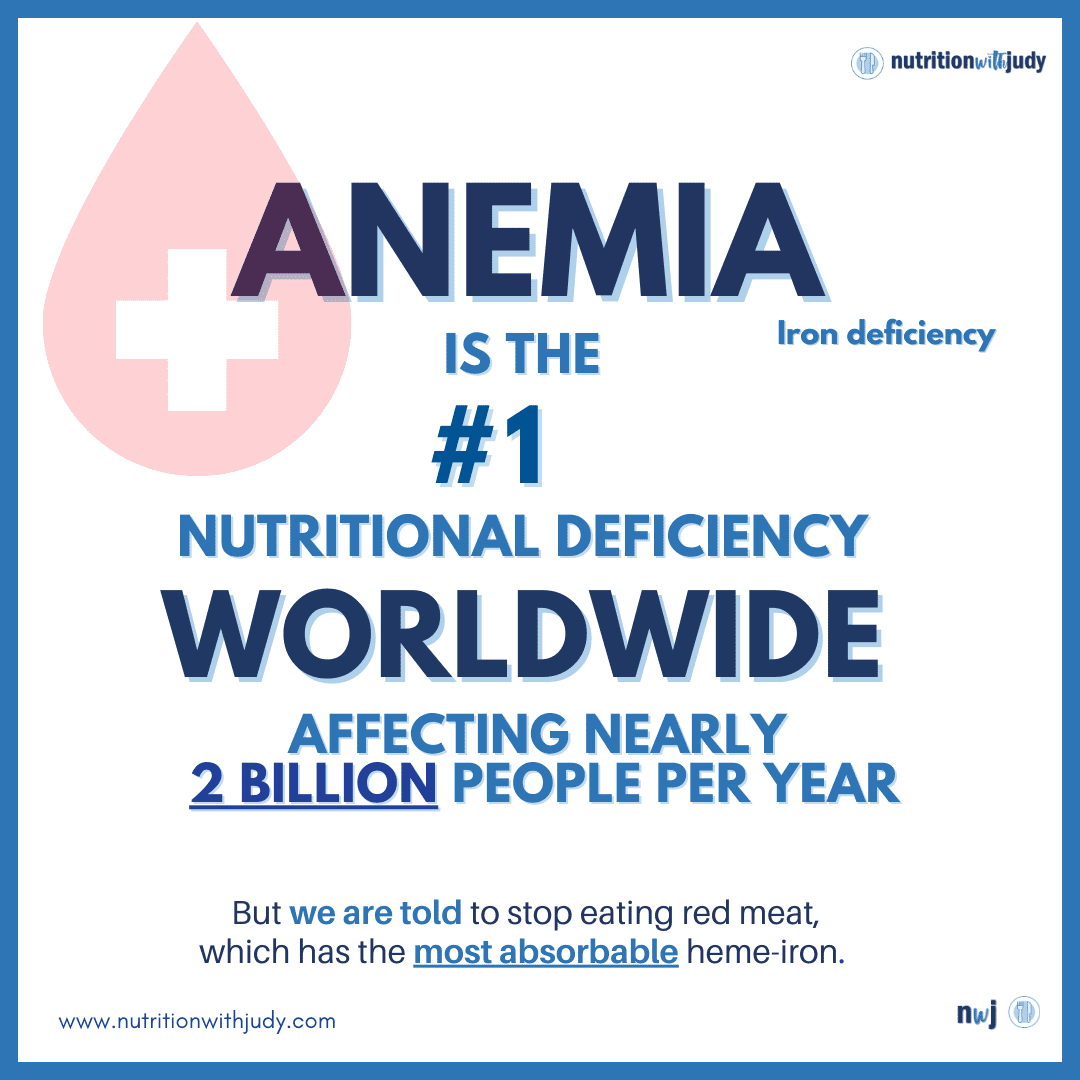
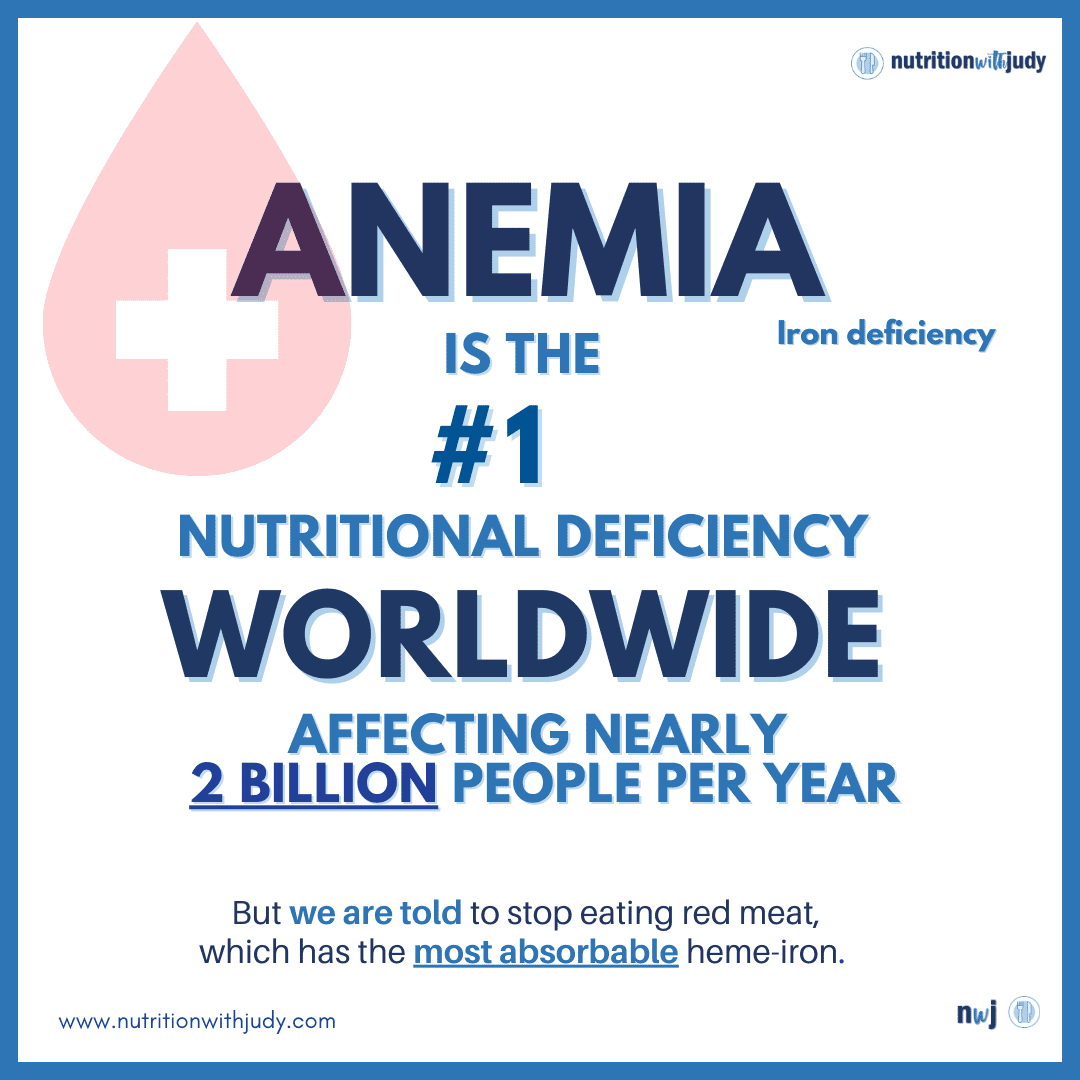
Iron-deficiency anemia (IDA) is the most common type of anemia and is the number one nutritional deficiency in the world. Iron is an essential dietary mineral used by red blood cells. It is a crucial part of hemoglobin, a protein found in red blood cells. Bone marrow needs iron in order to make hemoglobin. Hemoglobin delivers oxygen to all of the body’s cells.
What Causes Iron-Deficiency Anemia?
There are several factors that are associated with IDA, including:
- Lack of iron in the diet
- Menstruation
- Experiencing physical trauma or injury with blood loss
- Recent major surgery
- Blood loss from chronic nosebleeds, gastrointestinal (GI) disease, or kidney/bladder disease
- Donating blood frequently
There are also additional factors that can increase your risk of developing IDA:
- Heavy menstruation
- Breastfeeding
- Being pregnant or having a baby recently
- GI diseases
- Peptic ulcers
- Eating a vegetarian or vegan diet
- Heart failure
- Recently undergoing bariatric surgical procedures (e.g., gastric bypass)
Who Is Most At Risk for Iron-Deficiency Anemia?
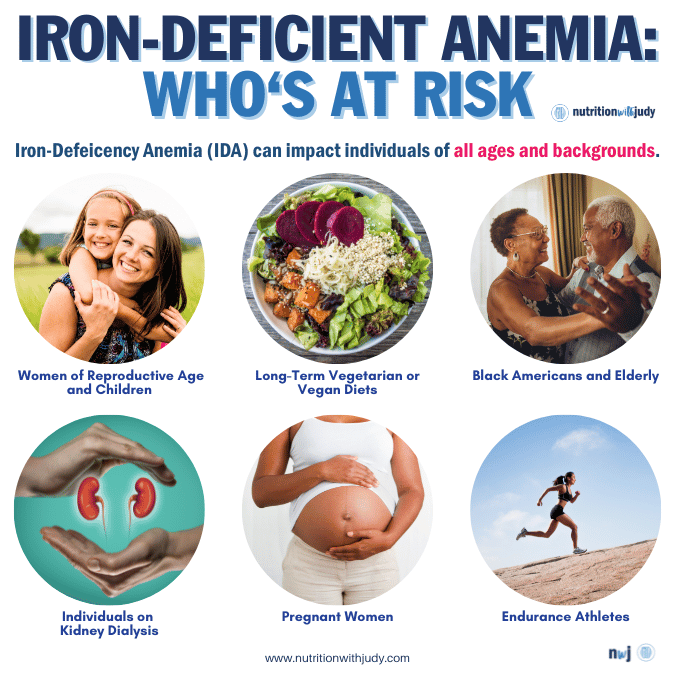
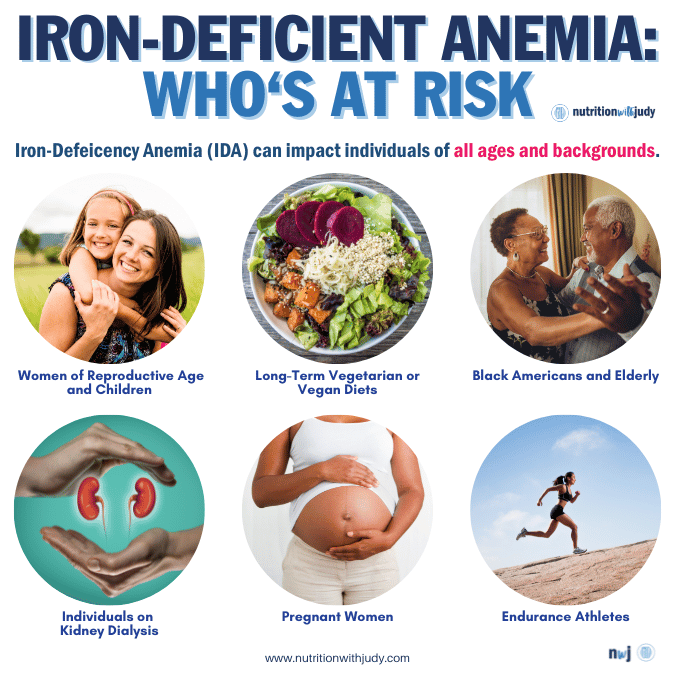
Anemia can impact individuals of all ages and backgrounds. However, women of reproductive age and children account for the largest percentage of IDA cases. While women are most likely to develop IDA, people who eat a vegetarian or vegan diet long-term have an increased risk of developing this condition. Vegetarian and vegan diets lack bioavailable iron (we’ll go more in-depth about this further in the article) as heme iron is only naturally occurring from animal sources. In terms of ethnicity, Americans of non-Hispanic Black descent are more likely to develop IDA. Research shows that anemia is 3.3 times more common in Black Americans than in Caucasians— the definitive reasons are unclear but the nuance is believed to be among differing demographic variables, socioeconomic factors, and comorbid conditions.
The following populations are also at a higher risk:
- Pregnant and menstruating women
- Elderly
- Individuals with kidney dialysis
- Endurance athletes
The Symptoms of Iron-Deficiency Anemia
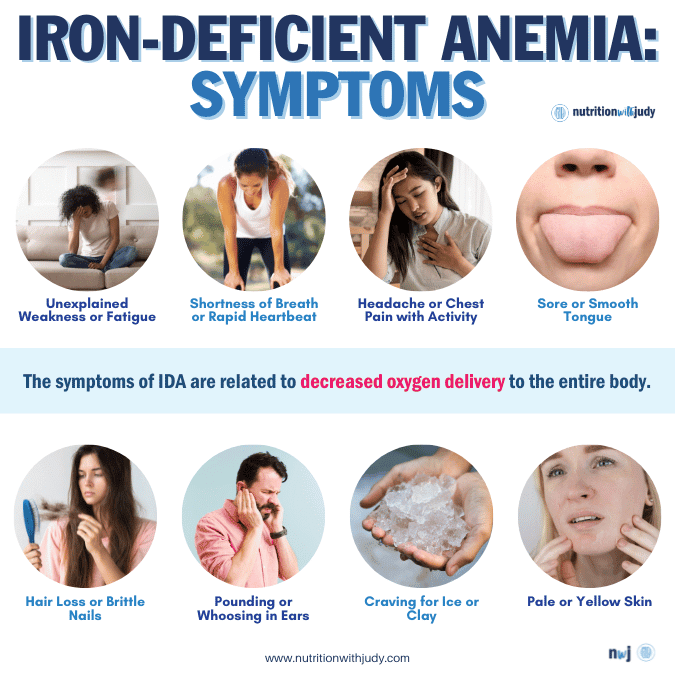
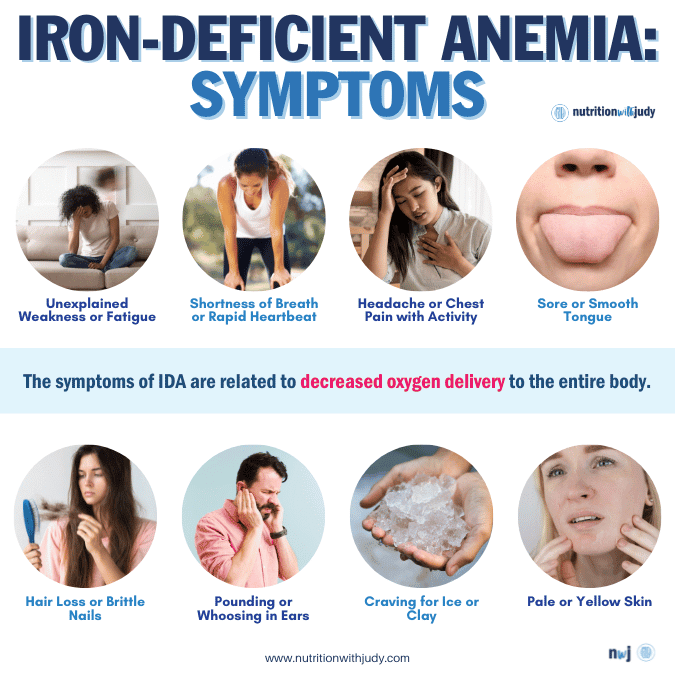
The symptoms of IDA are related to decreased oxygen delivery to the entire body. These symptoms include:
- Unexplained fatigue
- Unexplained general weakness
- Being pale or having “sallow” yellow skin
- Shortness of breath
- Chest pain, especially with activity
- Pounding or “whooshing” in the ears
- Rapid heartbeat
- Craving for ice or clay (e.g., pagophagia)
- Sore or smooth tongue
- Headache, especially with activity
- Hair loss
- Brittle nails
How Do You Test for Iron-Deficiency Anemia?
Left untreated, IDA can lead to frequent infections from a weakened immune system, heart failure, and pregnancy complications. Screening and early detection are essential for preventing further issues from developing.
IDA is diagnosed by blood tests, including a complete blood count (CBC). Providers may order additional tests to evaluate your levels of serum iron, ferritin, transferrin, and/or total iron-binding capacity. Individuals diagnosed with anemia from iron deficiency generally have the following results:
- Low serum iron (FE)
- Low ferritin
- High transferrin or total iron-binding capacity (TIBC)
- Low hemoglobin (Hg) and hematocrit (Hct)
- Low mean cellular volume (MCV)
- Low iron saturation
Additional tests may include:
- Peripheral smear: This blood test examines red and white blood cells and blood platelets. In IDA, the peripheral smear may show small, oval-shaped cells that appear to have pale centers.
- Fecal occult blood test: Practitioners may test for blood in your stool.
- GI abnormalities: An upper and lower endoscopy, capsule enteroscopy, barium enema, barium swallow, or small bowel biopsy may also be performed, depending on your medical history.
- Urine test: Testing the urine for blood or hemoglobin.
- Gynecologic evaluation: For women with increased or abnormal menstrual blood loss, a pelvic ultrasound or uterine biopsy may be performed.
How Do You Treat Iron-Deficiency Anemia?
Standard care acknowledges that increasing iron from food sources is one of the ways to improve iron intake. However, the main treatment approach is taking medicinal iron until the deficiency has been corrected and all iron stores have been replenished. In certain cases where iron deficiency can’t be corrected, standard care recommends ongoing iron supplementation.
Medicinal Iron and Supplements
Medicinal iron refers to prescription iron supplements with a higher amount of iron. There are several types of iron supplements, such as ferrous sulfate, ferrous fumarate, and ferrous gluconate. Intravenous iron is also available in different preparations, including iron dextran, iron sucrose, and ferric gluconate, but some individuals may have an allergic reaction. To add to the confusion, there are two numbers you’ll need to consider with iron supplementation: the chemical compound and the elemental numbers. Elemental iron is the most important number because it’s the amount available for absorption.
There are many issues with supplementing iron. The most common side effects are GI-related and include nausea/vomiting, diarrhea or constipation, flatulence, metallic taste, teeth staining, and epigastric distress. High levels of iron are also potentially toxic and can lead to iron poisoning and hereditary hemochromatosis. Since the body tightly regulates iron levels, a gradual build-up of iron in the body, also known as iron overload, can increase the risk of cancer, infection, and more. Individuals exploring the supplementation route will need to be very mindful of monitoring and managing their iron intake for these reasons.
Plant Food Iron Sources
Since standard care has demonized red meat and insists on limited overall meat in the diet, plant food sources are often recommended for increasing iron intake. Plant foods such as leafy greens, legumes, and iron-enriched grains are being pushed to increase iron levels. However, it’s important to note that there are two forms of iron available from food sources. Heme iron is only found in animal foods, while non-heme iron is found in plant foods. Heme iron from meat is better absorbed by the body than non-heme iron. More than 95% of functional iron in the human body is in the form of heme— that’s why heme is essential for our bodies.
Bran fiber, large doses of calcium, especially with supplementation, and plant compounds such as phytates and tannins can inhibit the absorption of non-heme iron. So not only is non-heme iron not as bioavailable to begin with, but you’ll also need to consider other components in your diet and supplementation that further inhibit absorption.
The Carnivore Diet for Iron-Deficiency Anemia
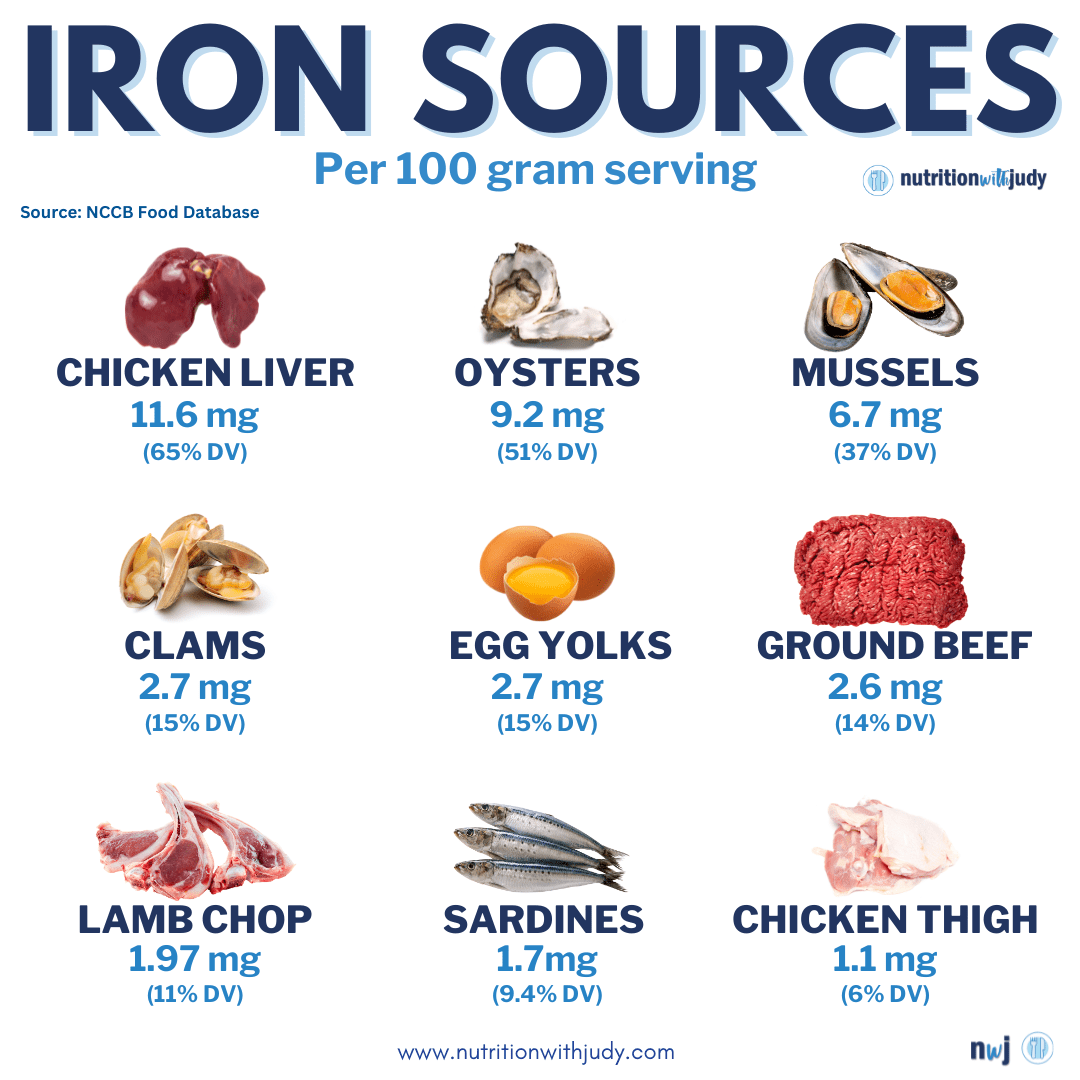
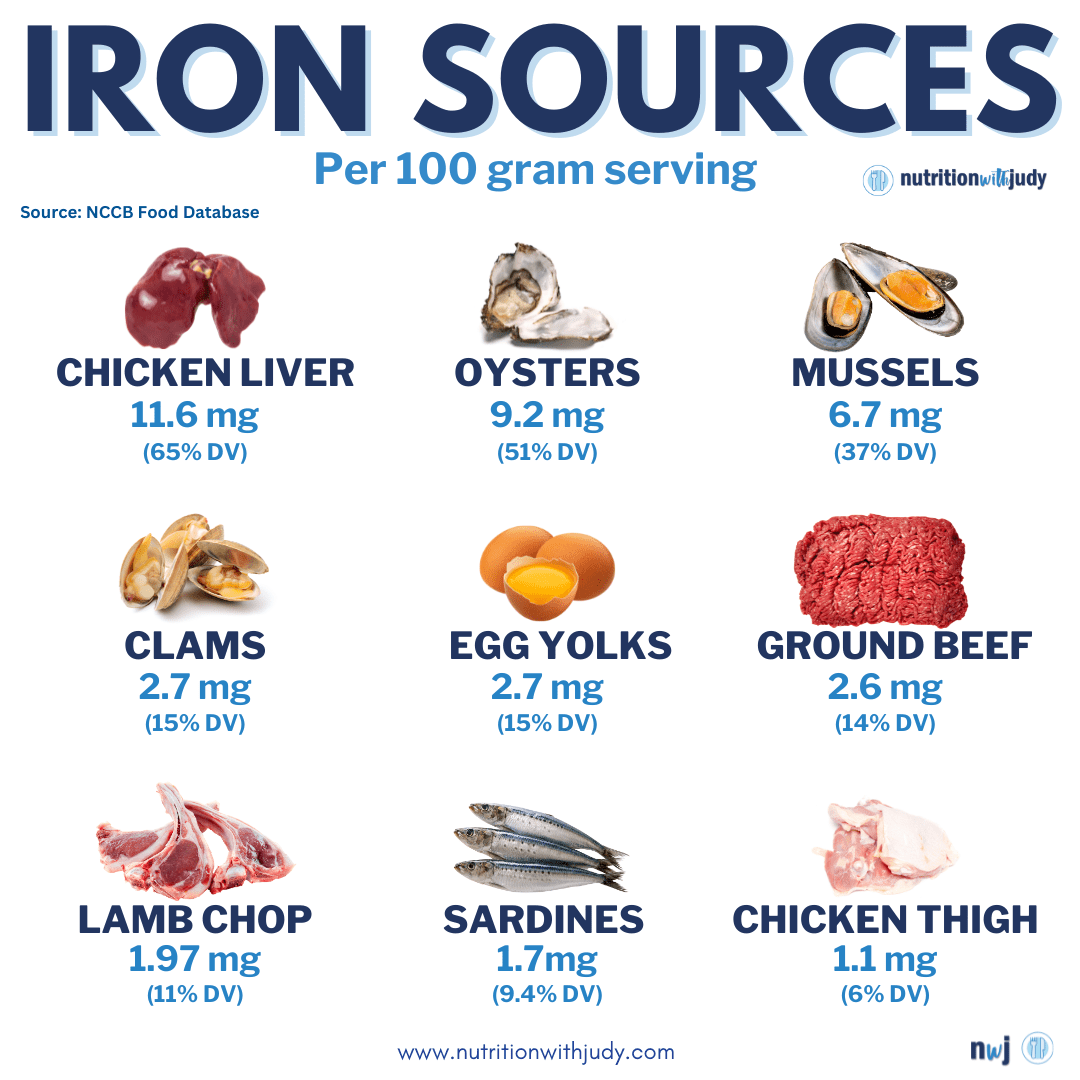
For those with IDA, a carnivore diet or meat-based diet is the best therapeutic approach for root-cause healing. It delivers bioavailable, iron-rich, nutrient-dense foods to help address any nutrition deficiencies, including iron. The carnivore diet is also rich in vitamin B12 and has safer options for folate, such as eggs, lamb chops, and chicken liver. While some may be concerned about folate deficiency with carnivore diets, we’ve debunked this issue here. Getting enough B12 and folate is another preventative measure against vitamin deficiency anemia.
Certain conditions such as GI disorders and peptic ulcers are associated with developing IDA— the carnivore diet offers powerful gut healing properties for supporting these and other chronic conditions. Eating a rainbow of meats is essential for proper nutrition and preventing potential nutrient deficiencies.
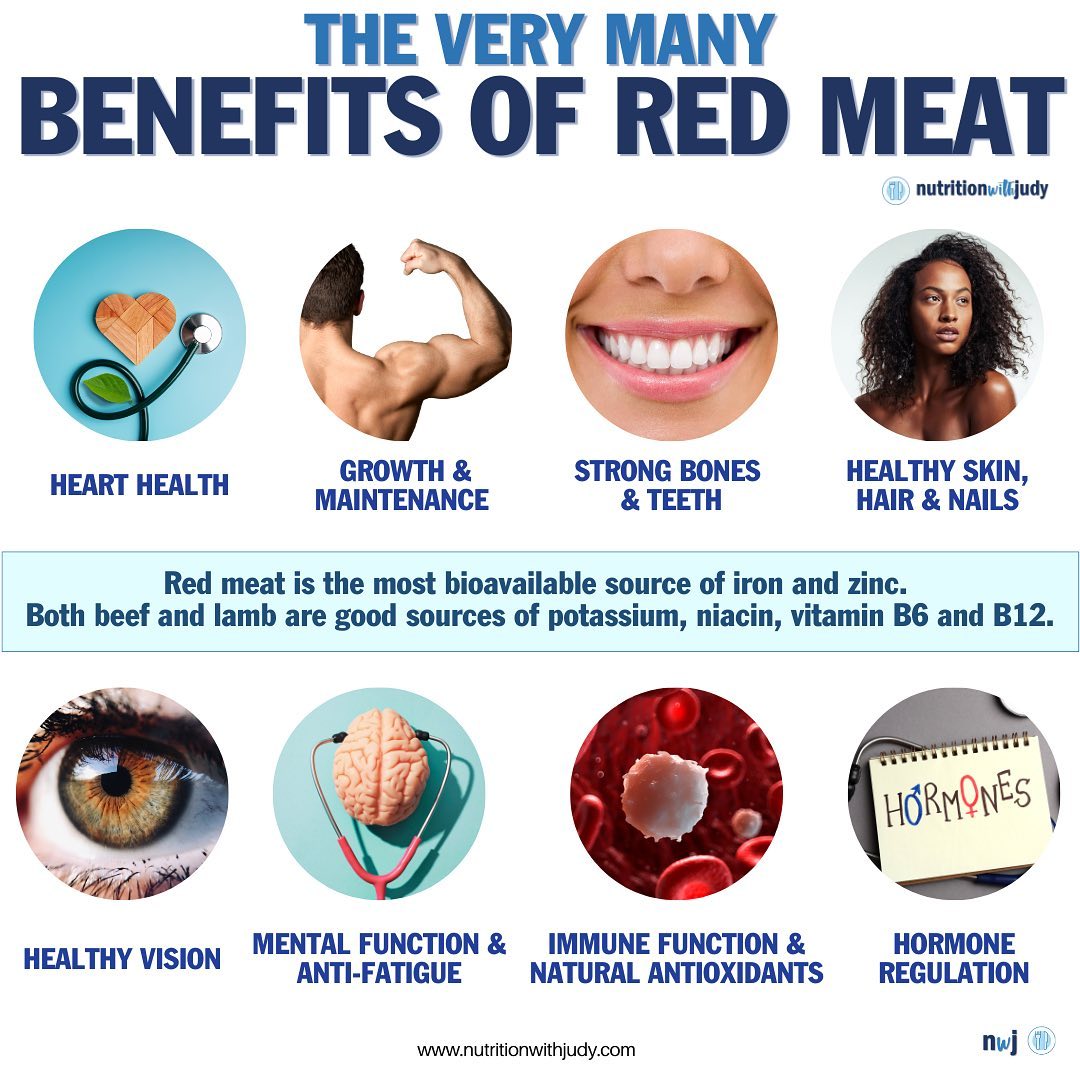
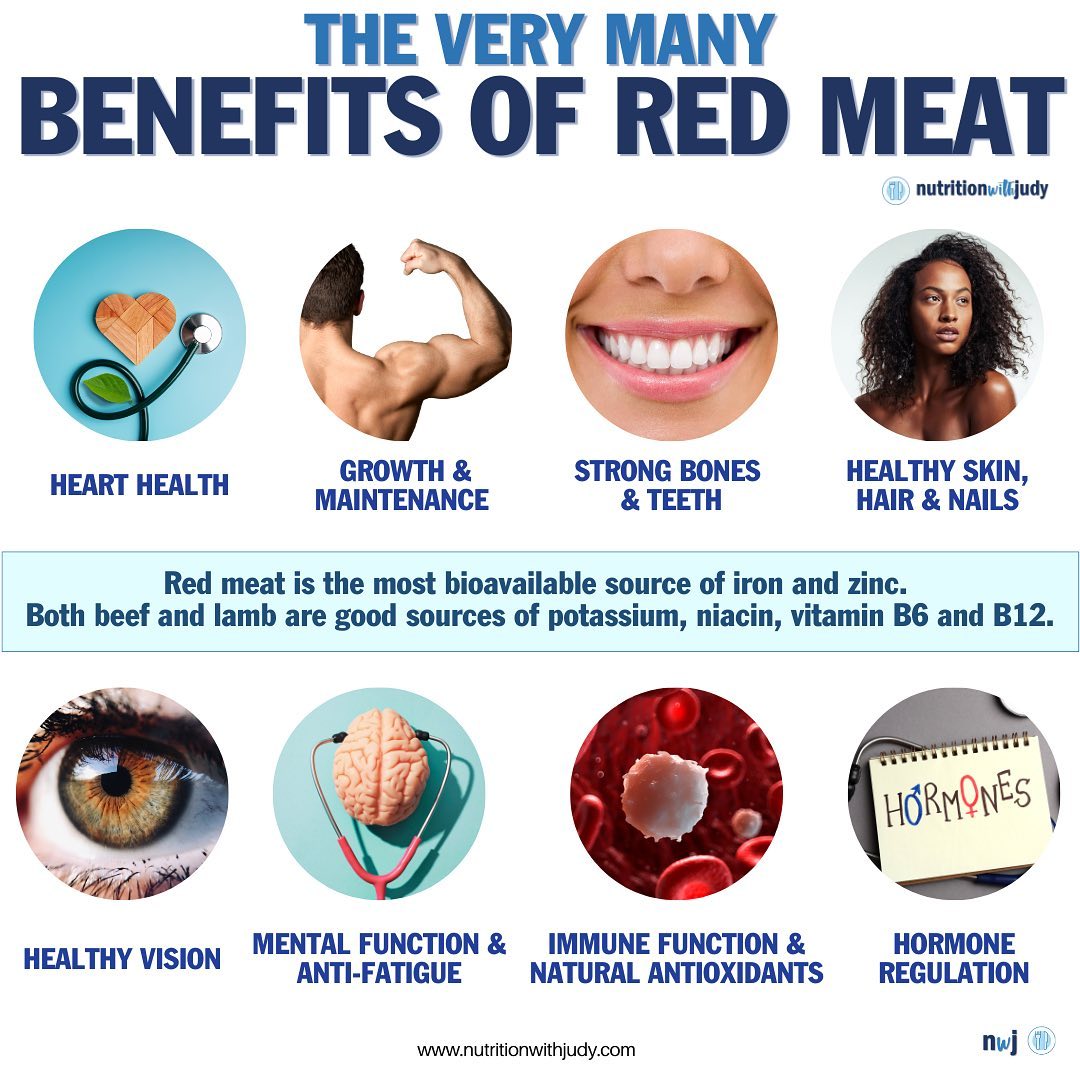
There are many reasons why individuals gravitate towards the carnivore diet. While it’s a proven therapeutic modality, you don’t have to go carnivore in order to prevent developing IDA. Red meat does help with anemia and is a superfood. But as you can see from the graphic above, there are many other animal sources for iron. A diet including plenty of meat is the best source of elemental heme-iron.
The Carnivore Diet and Excess Iron Concerns
For those who are on the carnivore diet and may be concerned with getting too much iron, we have yet to see a meat-based patient with iron overload or toxicity where dietary iron is the root cause issue.
High Ferritin Levels
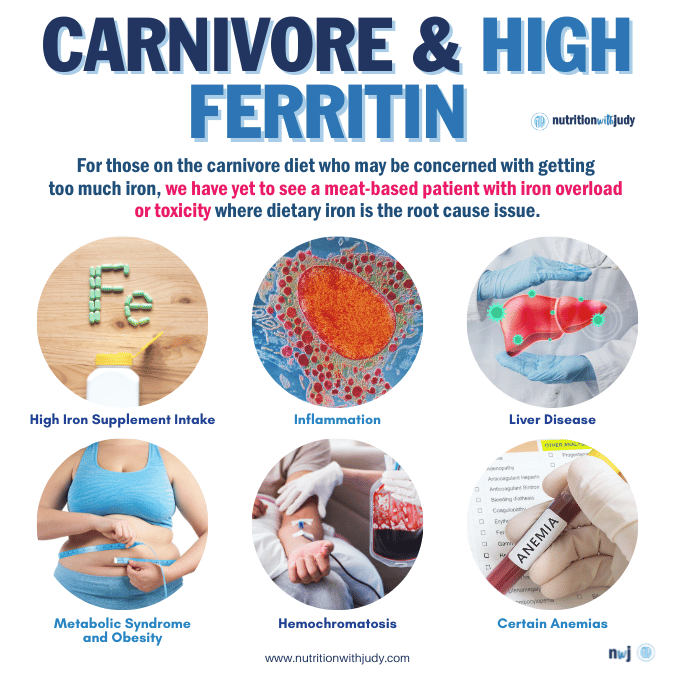
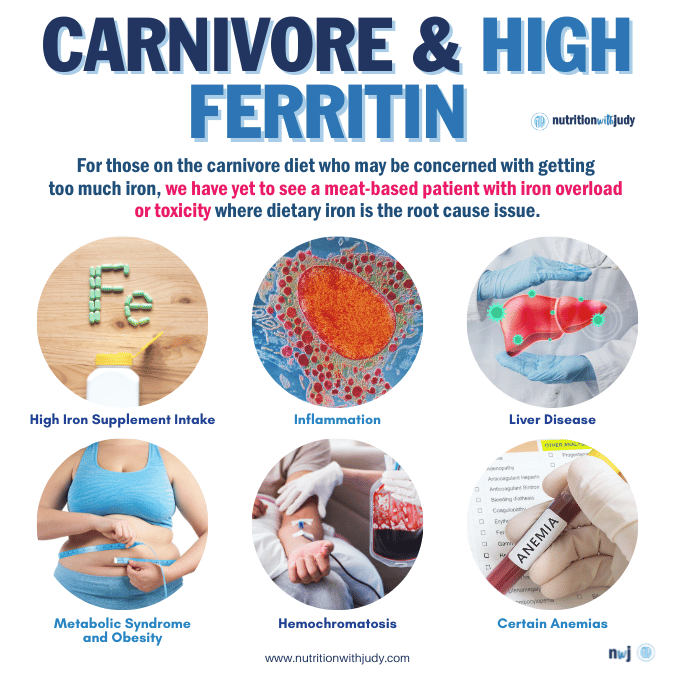
Ferritin is a protein that stores iron and releases it in a controlled manner. It’s found in the body’s cells, with the highest concentrations in the liver, spleen, and bone marrow. Ferritin is essential because it helps maintain a balance of iron in the body, which is crucial for many bodily functions, including the production of red blood cells. If there is not enough iron in the blood, ferritin ideally releases the iron in storage. Sometimes excess ferritin is seen in our clients but it’s not due to meat consumption.
The following are some reasons for high ferritin (the storage form of iron):
- High Iron Intake: Consuming too much iron, especially through supplements, can increase ferritin levels. This is more common in people who take high-dose iron supplements.
- Inflammation: Since ferritin is also an acute phase reactant, levels can increase in response to inflammation or infection. This is a way for the body to sequester iron from bacteria that need it to grow.
- Liver Disease: Conditions such as alcohol-related liver disease, non-alcoholic fatty liver disease, and hepatitis can lead to increased ferritin levels.
- Certain Anemias: Although it might seem counterintuitive, some types of anemia, such as anemia of chronic disease or sideroblastic anemia, can cause elevated ferritin levels.
- Hemochromatosis: This genetic disorder causes the body to absorb too much iron. The excess iron is stored as ferritin in various organs, particularly the liver, and can lead to organ damage.
- Metabolic Syndrome and Obesity: These conditions are sometimes associated with elevated ferritin levels, likely due to low-grade systemic inflammation.
To manage and reduce high ferritin levels, it’s important to identify and address the underlying cause. This might involve reducing supplementary iron intake, phlebotomy (blood removal) in conditions like hemochromatosis, or treating underlying root-cause inflammation or liver disease.
Regularly monitoring ferritin levels and iron status is critical in managing these conditions.
Closing Thoughts On Iron-Deficiency Anemia
The easiest way to prevent IDA is by making sure meat is at the center of your diet. While other factors can increase your risk of developing IDA, eating a heme iron-rich diet to ensure your iron stores have healthy levels is critical.
If you have IDA, rather than worrying about all the nuance involved with iron supplementation, eat meat instead.
Work With Our Trusted Carnivore Diet Functional Nutritional Therapy Practitioners
The Nutrition with Judy practice is honored to be a trusted carnivore diet practitioner support serving clients from around the globe. We’re passionate about helping our clients achieve root-cause healing in order to lead the best quality of life possible that’s nearly symptom-free. Our team is dedicated to educating our community about the incredible benefits of the carnivore diet. We welcome you to explore our free resources and are always available to support you through personalized protocols. Our Symptom Burden Assessment (SBA) is the perfect starting point for discovering your root cause and is required to work with our team— you can learn more in-depth about this powerful tool here.
Start your root-cause healing journey today and contact us any time with any questions or concerns.
DISCLAIMER: This content is for educational purposes only. While we are board-certified in holistic nutrition and are nutritional therapy practitioners, we are not providing medical advice. Whenever you start a new diet or protocol, always consult with your trusted practitioner first.


Lee
January 20, 2024 at 7:23 amFinally some information about high Ferritin – mine just tested 313. I’m being tested for Hemochromatosis, but it’s unlikely. Someone suggested I stop using cast iron skillet to cook my meat; somebody else suggested I become a regular blood donor. Thank you for this article!