How Fructose From Excess Fruit Causes Fatty Liver
The carnivore diet has been leveraged as a powerful healing modality for various health conditions ranging from autoimmunity to gut healing. There are many different variations available with meat-based diets for individuals to choose from. One of these variations is called the “animal-based diet” which focuses on meat with the inclusion of dairy, fruit, and honey. While some proponents of this variation make claims that carbohydrates are essential for certain functions such as hormone production and electrolyte balancing, we beg to differ. One of the concerns with adding fruit to any diet is the potential for fatty liver disease. Regardless of what diet you’re on, fructose may cause fatty liver. Let’s take a closer look at how the body metabolizes fructose, why fructose can be problematic, and the risks of fatty liver.
What Is Fructose?
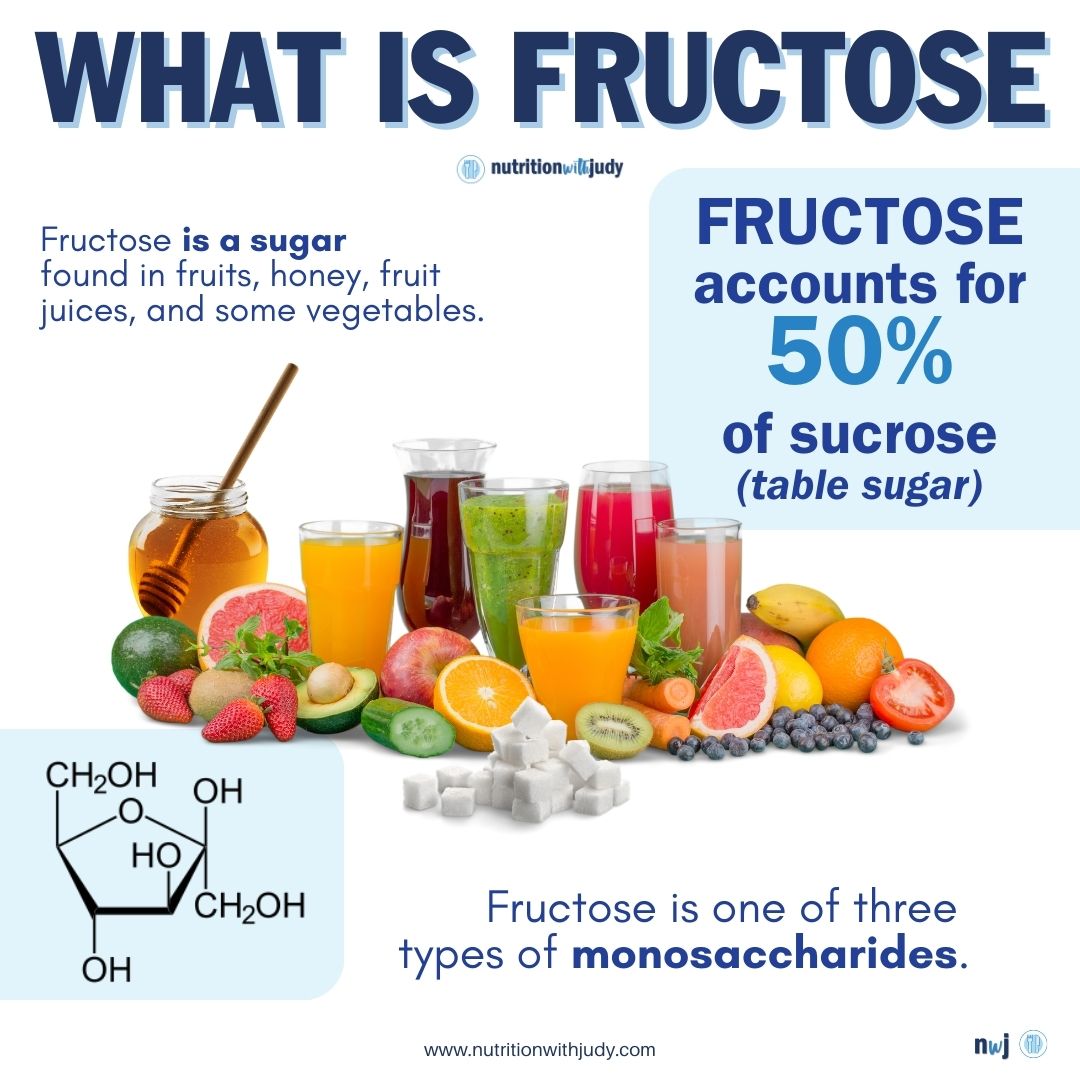
Fructose is a sugar found in fruits, honey, fruit juices, and some vegetables. It belongs to a group of monosaccharides. Monosaccharide is the simplest form of sugar. It is the basic unit from which all carbohydrates are built. There are three types of monosaccharides: fructose, galactose, and glucose. Fructose accounts for 50% of sucrose (table sugar).
French chemist Augustin-Pierre Dubrunfaut discovered fructose in 1847. However, German Nobel laureate Emil Fischerwas the one who conducted pioneering research on fructose and all other known sugars at the time. Fischer worked on his research from 1884 to 1894.
As the most water-soluble monosaccharide, fructose dissolves in exceedingly small amounts of water.
How Does the Body Break Down Fructose?
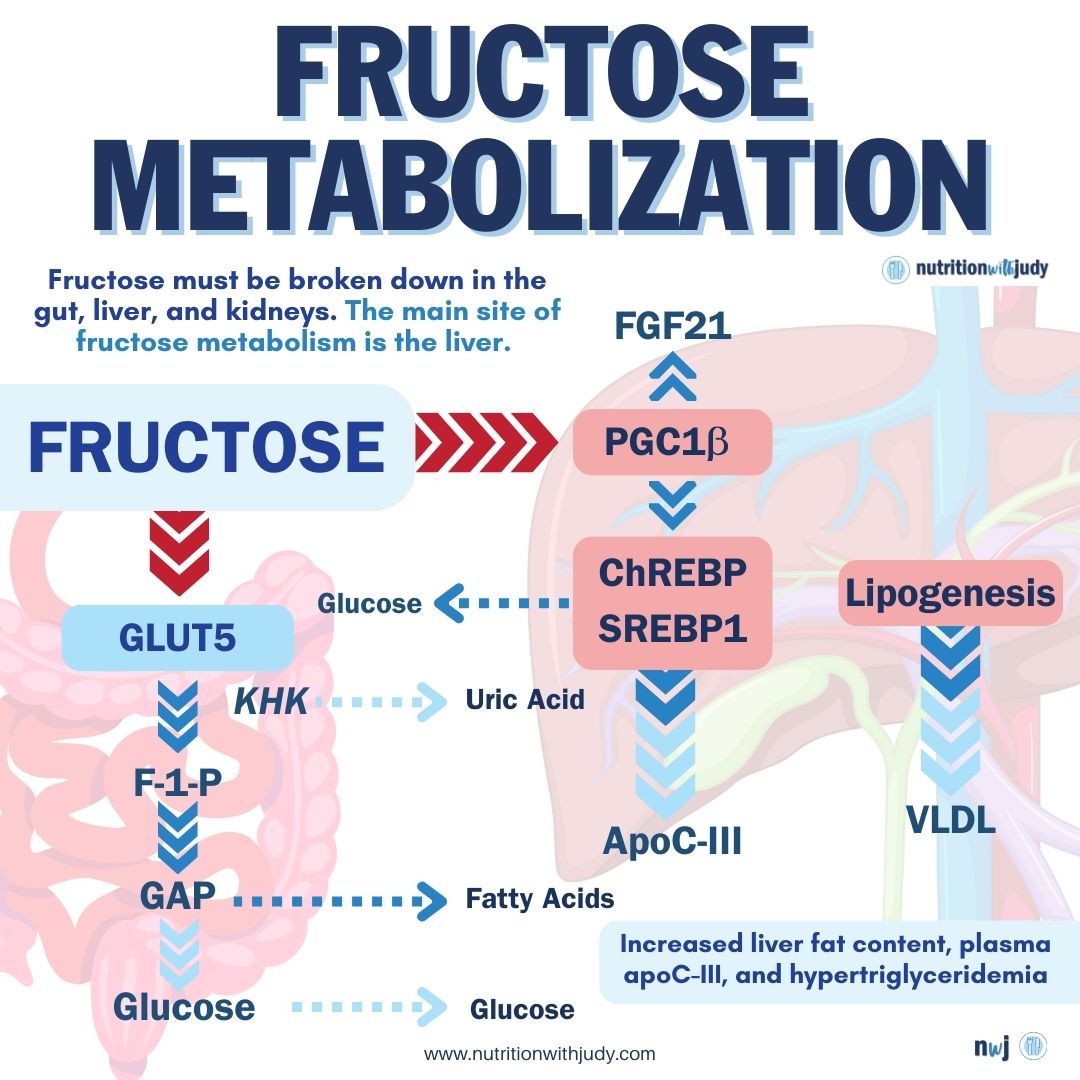
Most cells in the body can’t metabolize fructose directly. Instead, fructose needs to be broken down in the gut, liver, and kidneys. The main site of fructose metabolism in the body is the liver. In the liver, fructose enters the intermediary pathways of the metabolism of carbohydrates. The liver readily extracts fructose thanks to the presence of an active hepatic enzyme system for breaking down fructose. The biggest part of the ingested fructose is eliminated in a single pass through the liver. For that reason, upon consumption of moderate levels of fructose-containing foods, the concentration of this fruit sugar in the blood is low.
In the liver, fructose enters hepatocytes (liver cells) and goes through a process of phosphorylation. During this process, the fructose molecule gets a special tag in the form of a phosphate group to make a fructose derivative called fructose-1-phosphate. This allows the liver to work with fructose more easily. In order to perform this important process of phosphorylation, the liver recruits an enzyme called ketohexokinase (KHK-C). The liver also needs a molecule called adenosine triphosphate (ATP) that provides energy. Another enzyme, called fructokinase, supports the whole process of phosphorylation to break down fructose.
After phosphorylation, an enzyme called aldolase B cuts the fructose-1-phosphate into two parts. These two parts are called dihydroxyacetone phosphate (DHAP) and glyceraldehyde. DHAP is like a building block used for the purpose of glycolysis, the process where sugar is turned into energy. So, when you eat food that contains fructose (e.g. fruits) the levels of glucose in the blood increase. This happens because fructose is converted to glucose.
Glyceraldehyde also gets the “special tag” through the process of phosphorylation. The enzyme triokinase adds that tag to make glyceraldehyde-3-phosphate (also known as triose phosphate), which is a versatile building block. The newly formed compound can be used to produce glycogen (a storage form of glucose) or to create fatty acids and more glucose. The development of the triose phosphate compound marks the transition from fructose to glucose.
The process of metabolizing fructose in the body is similar to that involved in the breakdown of glucose. The main difference is that glucose is metabolized directly throughout the body. But, fructose is broken down primarily in the liver.
What Is Fatty Liver?


Fatty liver is a condition that results from excessive fat accumulation in the liver. A healthy liver contains a little bit of fat. However, it becomes a problem when fat content is about 5% to 10% of the total weight of the liver. There are two types of fatty liver:
- Alcohol-induced fatty liver disease: Occurs due to regular, heavy alcohol intake. The prevalence of this disease in U.S. adults is 4.3% to 4.7%, according to a report from JAMA. While generally asymptomatic, alcohol-induced fatty liver disease is a warning sign that indicates a person’s alcohol intake is at a harmful level. The disease can be reversed if a person stops drinking.
- Non-alcohol-related fatty liver disease (NAFLD): The buildup of fat in the liver occurs due to a wide range of other factors such as being overweight and obese, insulin resistance, high blood sugar, and high levels of fats (especially triglycerides) in the blood. The prevalence of this disease in North America ranges from 35.3% to 47.8%. The global prevalence of NAFLD is 32% and it is more common in men than women.
Everyone can develop fatty liver, but some people are at a higher risk. Common risk factors include Hispanic or Asian descent, postmenopausal age, obesity, hypertension, diabetes, high cholesterol, and obstructive sleep apnea. Alcohol used to be the main risk for fatty liver, but other compounds and foods in our diet can also lead to this problem. Fructose is an excellent example.
Fructose and Fatty Liver
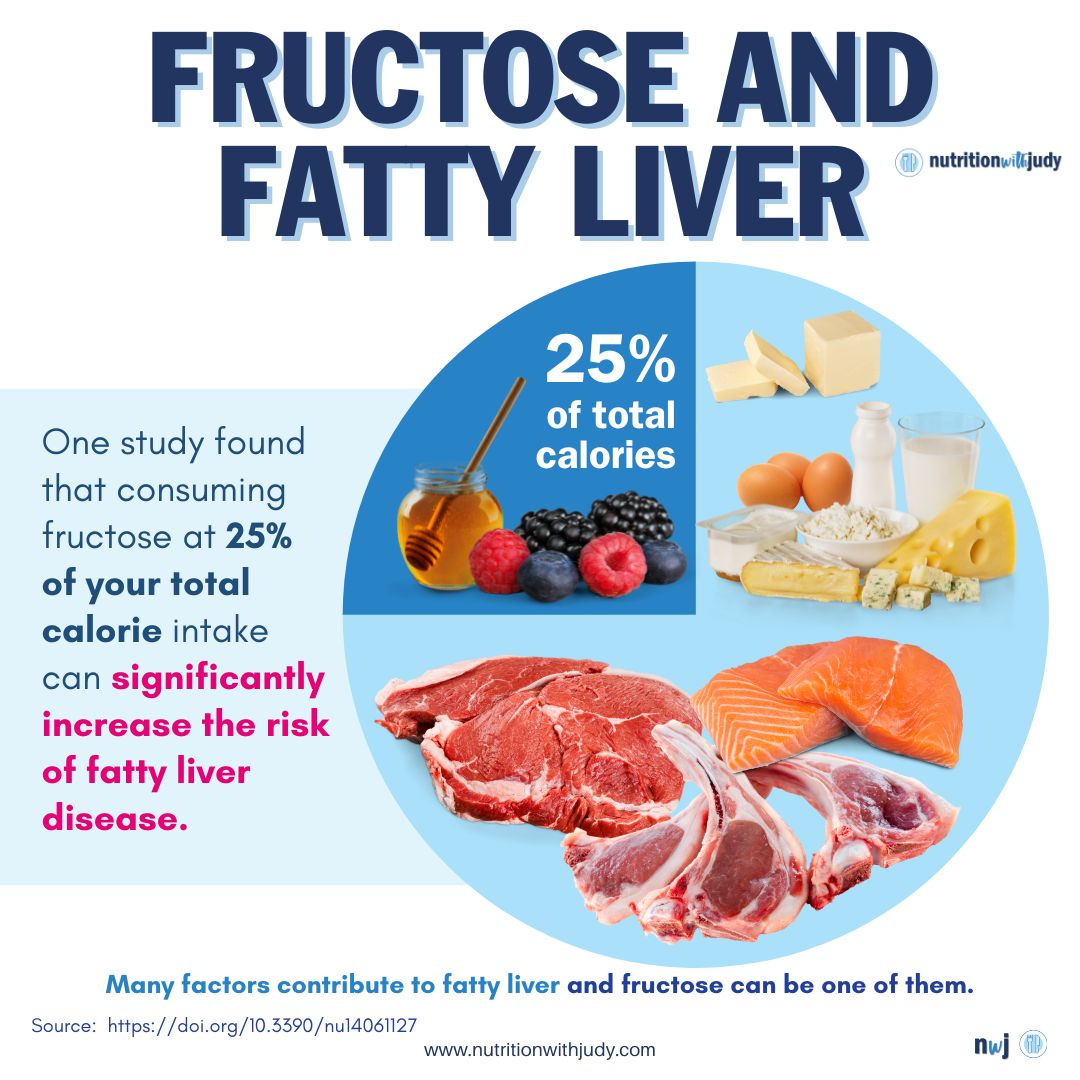
Various factors contribute to the onset of fatty liver, and fructose could be one of them. The March 2022 issue of Nutrients published a review of the involvement of fructose in fatty liver and potential mechanisms of action. The review showed that added fructose regulates physiological mechanisms and promotes the accumulation of fat in the liver. Consumption of fructose equal to 25% of the total caloric intake may increase hepatic lipogenesis (the process where the liver creates new fat molecules). In people with NAFLD, higher consumption of fructose per day was strongly connected to a reduction in high-density lipoprotein (HDL). At the same time, fructose intake in patients with NAFLD was linked to higher severity of fibrosis and liver inflammation.
The same review describes that a diet high in fructose promotes stimulation of de novo lipogenesis (DNL) due to higher upregulation of transcription factors. De novo lipogenesis is a process wherein carbs from circulation are converted into fatty acids and used to synthesize other lipid molecules such as triglycerides. The result of DNL induction is that when fructose is broken down in the body, some of the leftover substances contribute to the production of fat molecules. Moreover, fructose supports the production of malonyl CoA, a molecule in the synthesis of fatty acids. This inhibits the oxidation of fatty acids and leads to a buildup of triglycerides in the liver. The main problem here is that the buildup of fat causes liver problems such as fatty liver diseases and jeopardizes a person’s health and well-being. Chronic intake of fructose impairs the balance of the intestinal microbial flora, which can also contribute to inflammation of the liver and the onset of NAFLD.
A comparative study from the February 2010 issue of the European Journal of Nutrition found that diets containing 30% fructose as free fructose and glucose or sucrose are associated with fatty liver.
The November 2013 issue of the International Journal of Molecular Sciences found that chronic intake of fructose is associated with various problems including NAFLD, even in the absence of obesity. While this study does include high fructose corn syrup (HFCS), it’s important to note that studies regarding fructose exclusively from fruit are quite limited and require more research to identify the underlying mechanisms of the effects of fruits on NAFLD. One study indicated that the consumption of fruits more than four servings per day exacerbated steatosis, glycemic control, and dyslipidemia in NAFLD patients.
The only other controlled trial completed on fruit and NAFLD analyzed how patients with preexisting NAFLD fared with a fruit-rich diet. These individuals experienced increases in body weight, BMI, waist circumference, glucose, insulin, HOMA-IR, triglycerides, and liver enzymes compared to the control group without NAFLD. Researchers note that there is existing evidence linking high fructose intake with NAFLD, however, research has only been completed in the context of a hypercaloric diet with added fructose. It’s also noted that there were no differentiations made between what fruits participants were eating during this trial, even though the sugar content range is vast. Limes typically have 1.13 grams of sugar while one mango generally has 46 grams of sugar.
Fructose, Fatty Liver, and Children
Studies report that 5% to 10% of children have NAFLD in the US. NAFLD has become more and more common in recent decades alongside the rise of childhood obesity. The leading hypothesis for this change is the increased consumption of ultra-processed foods and sugar. Fructose is also believed to play a role in this. A recent study reported that each gram of daily fructose consumed at the age of 14 for obese adolescents was associated with a 9% increased risk of NAFLD at the age of 17. Fructose consumption has been directly linked to NAFLD development in obese children.
Another recent study found that adherence to a Mediterranean diet high in monounsaturated fatty acids and low fructose decreased liver inflammation and insulin resistance in pediatric patients with biopsy-proven NAFLD. The same study notes the importance of sugar addiction and its role in pediatric NAFLD cases.
Counter Fructose Studies
Since the research is quite limited when it comes to specifically fructose from fruit and fatty liver, let’s break down some of the studies used by pro-fructose advocates in the carnivore space.
This paper challenges the arguments against fructose. The paper argues that fructose consumption has not increased historically and that fructose may not be the problem. The paper also states that fructose isn’t ever found without glucose, so studies that isolate fructose aren’t real-life scenarios.
Dr. Richard Johnson and other researchers have done studies isolating the different forms of sugars as well as many studies in natural food forms.
Here are some thoughts from the conclusion:
“…Fructose is safe at typical intake levels but can produce adverse metabolic effects when abused- as is true of most nutrients. It turns out that the largest abusers of fructose are not American consumers, but research scientists…
Humans consume fructose with lots and lots of glucose; >5 times as much glucose as fructose…”
There is a lot of subjectivity written in this paper, calling research scientists abusers is a bit much, and why the reiteration of the word lots?
“Evidence is presented in this review that fructose has not disproportionately increased in the human diet (in fact, it has increased very little in the past 90 years) and that cause-and-effect evidence of adverse effects is lacking at typical human exposure levels and patterns. The fructose hypothesis must be continually challenged for human relevance…
Is it time for granting agencies and journal editors to require more physiologically relevant experimental designs and clinically important outcomes for fructose research? I think it is.”
Again, there is a lot of subjectivity in the paper and passive blame toward glucose. Dr. Richard Johnson and researchers have found that glucose and fructose can convert to one another via the polyol pathway. So why does it even matter?
Our bodies have these pathways so when there’s too little or too much of something, our body has ways to protect itself.
But here’s the biggest kicker…
This paper was presented at a symposium sponsored by the Corn Refiners Association and the main author is compensated and a consultant and advisor to the food and beverage industry in the area of nutritive sweeteners.
We’ll use the author’s words, is this paper abusive against fructose and could there be lots and lots of conflicting interests? We think so…
This paper should not have been shared as evidence-based research.
This was another paper shared by the pro-fructose advocate. We’ll let you see if you can figure out the issues. Let us give you a hint with a closer, highlighted look.
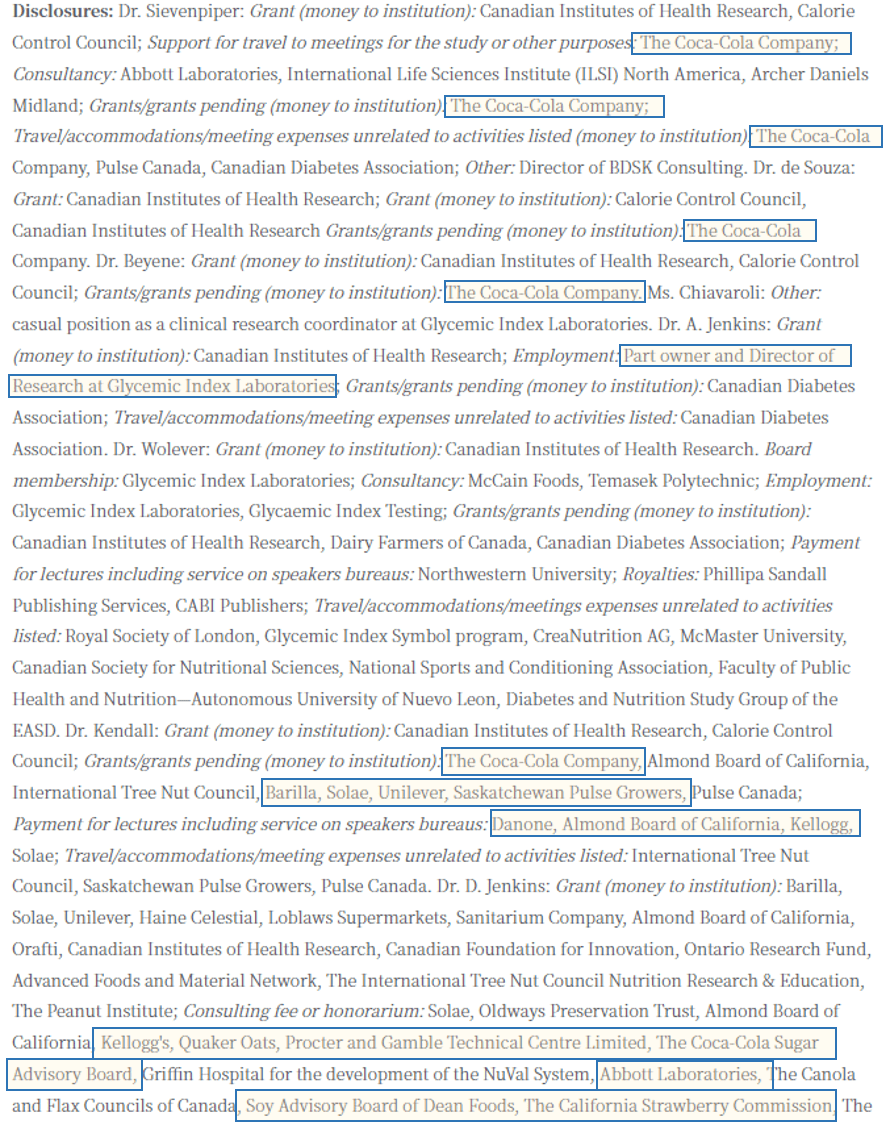
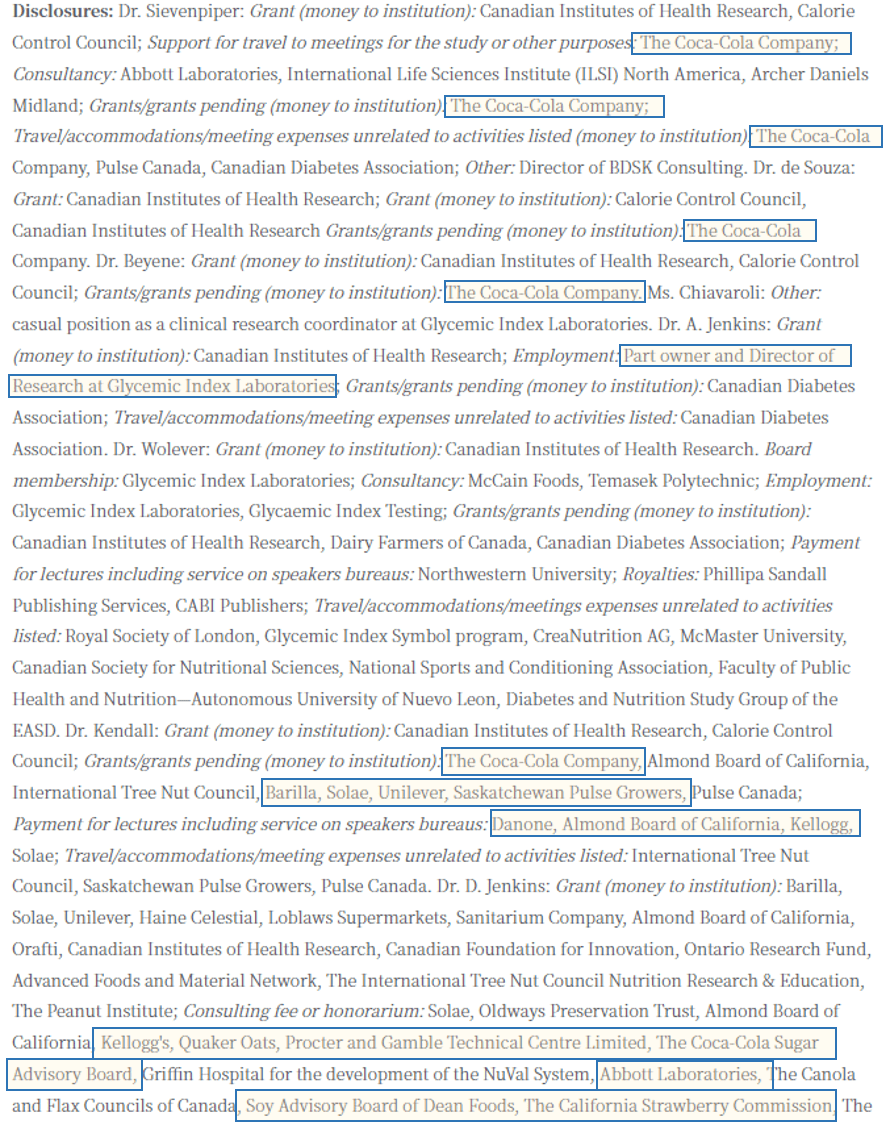
We really need to do better.
The other long fructose perspective does not deny that fructose is harmful. They essentially argue that the dose makes the poison. But for every single person, that dose will differ.
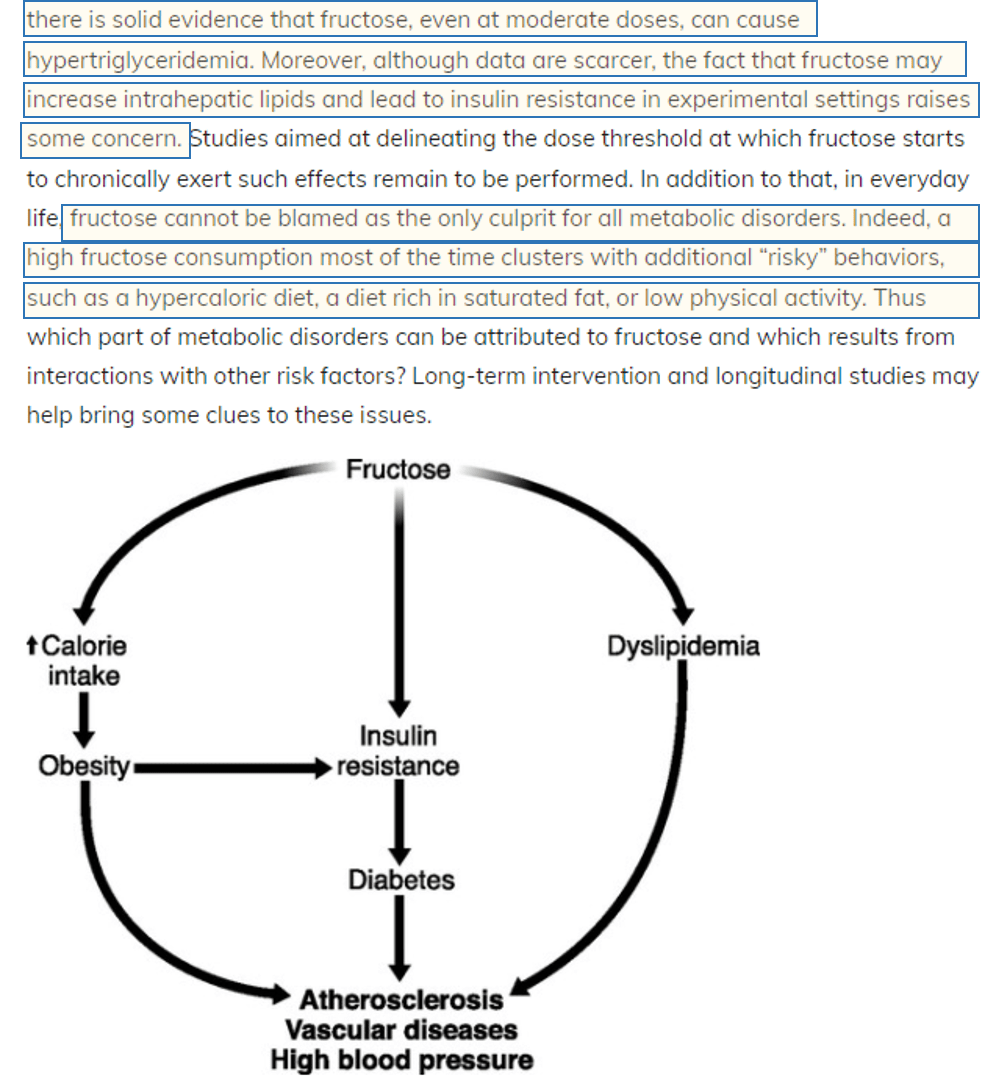
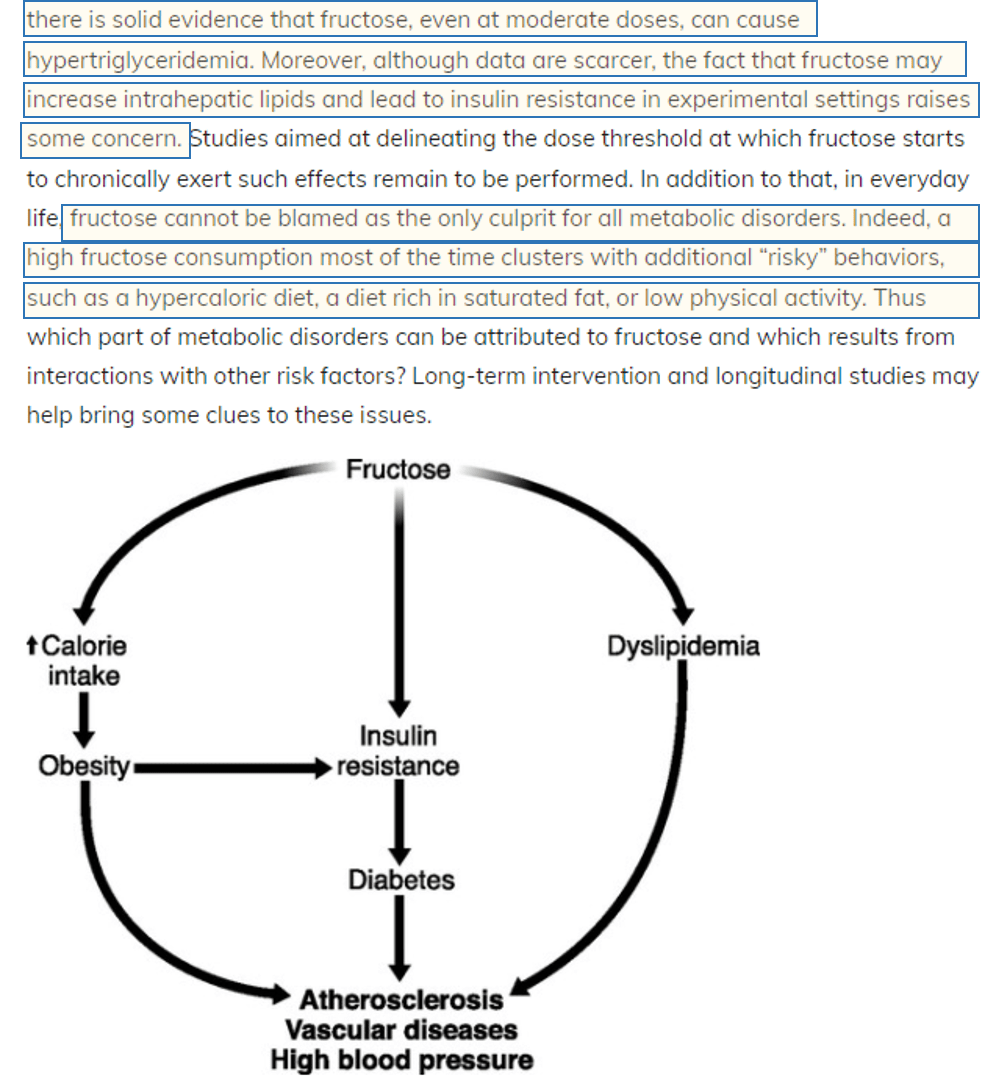
We cannot share studies where we agree with the author’s hesitation with fructose but do not necessarily agree with the author’s alternative suggestions. This author defines risky behavior as consuming saturated fats. The author mentions other metabolic disorder drivers (other than fructose) such as excess calories, diets rich in saturated fats, and/or low physical movement.
So if risky behavior is eating a diet rich in saturated fats and fructose, are we agreeing that fructose (fruit/honey) isn’t ideal on a meat-based diet?
Below is part of the conclusion.
We really need to dive into studies that are used to make a strong stance, especially ones that scare the community.
We don’t need carbs for optimal health.
Fructose Metabolism Is Similar to Alcohol Breakdown
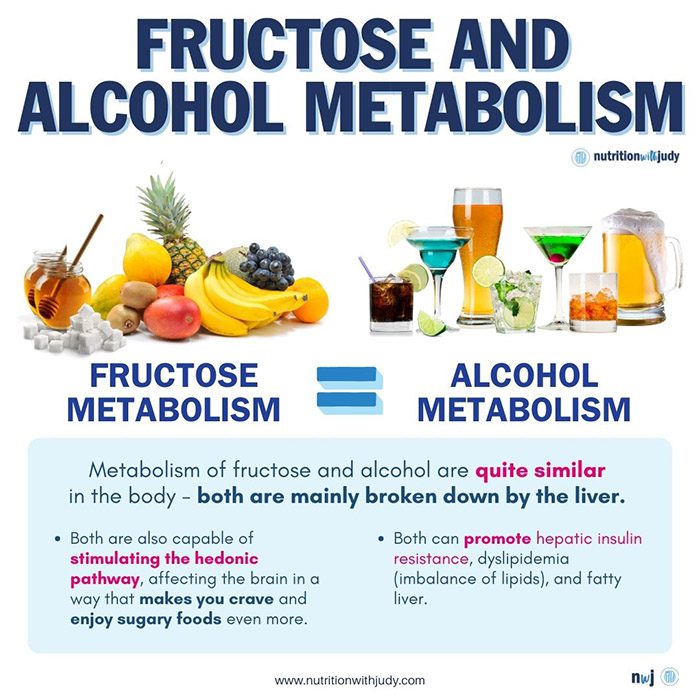
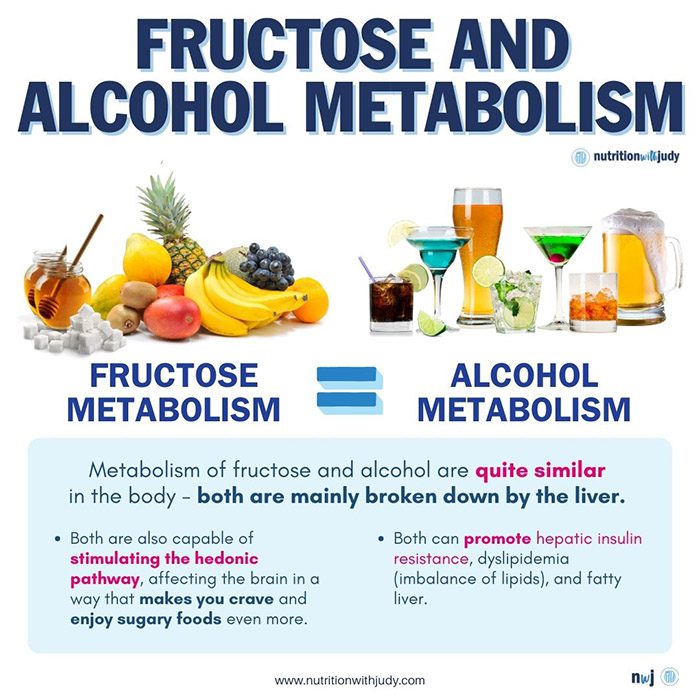
Metabolism of fructose is quite similar to the process that breaks down ethanol or alcohol in the body. For both fructose and alcohol, the main site of metabolism is the liver. Both compounds act as substrates for de novo lipogenesis. Also, fructose and alcohol alike promote hepatic insulin resistance, dyslipidemia (imbalance of lipids), and hepatic steatosis (fatty liver).
When proteins in the liver react with fructose and produce a substance called superoxide, a person may develop liver inflammation. This inflammation is quite similar to what happens when the liver metabolizes alcohol. It’s also useful to mention that fructose can stimulate the hedonic pathway in the brain both directly and indirectly, i.e. it affects the brain in a way that makes you crave and enjoy sugary foods even more. That’s why consuming too much fructose can become habit-forming and may result in dependence on sugary foods, similar to how some people become dependent on alcohol.
In small doses, neither fructose nor alcohol will overwhelm the hepatic mitochondrial capacity. The problem comes with higher doses and chronic intake. Fructose and alcohol drive DNL and generate intrahepatic lipids or buildup of fat inside the liver. They also contribute to inflammation in the liver and insulin resistance. Through these particular phenomena, the hepatic metabolic profile of fructose is similar to that of alcohol.
While more research on this subject is necessary, current evidence shows that both fructose and alcohol consumption are associated with increased fat content in the liver and development of fatty liver. A potential mechanism of action could be the suppression of insulin-signaling pathways which leads to the uncontrolled activation of a hepatic transcription factor SREBP1 c, which can contribute to fatty liver.
Fructose Contributes to Weight Gain and Results in Fatty Liver
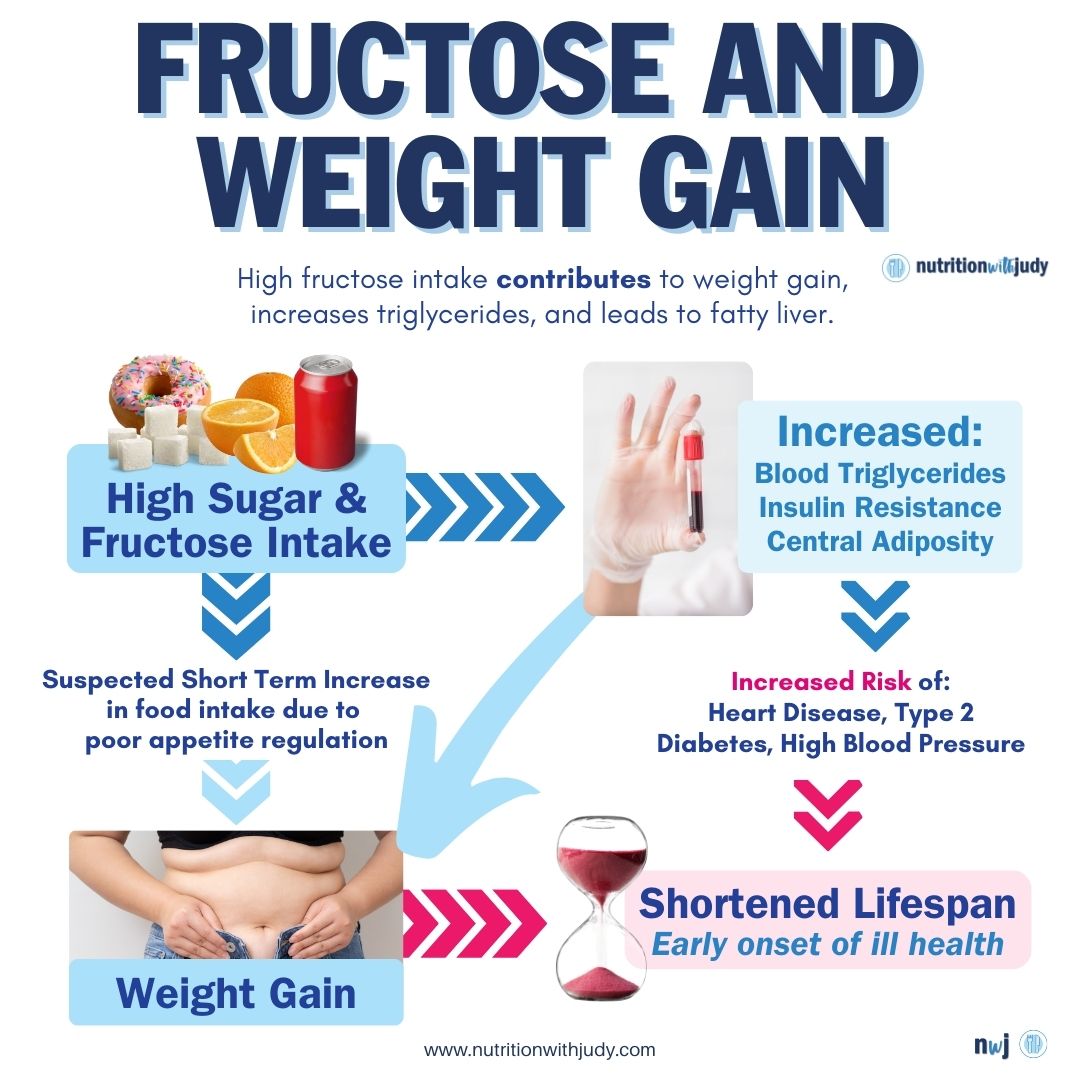
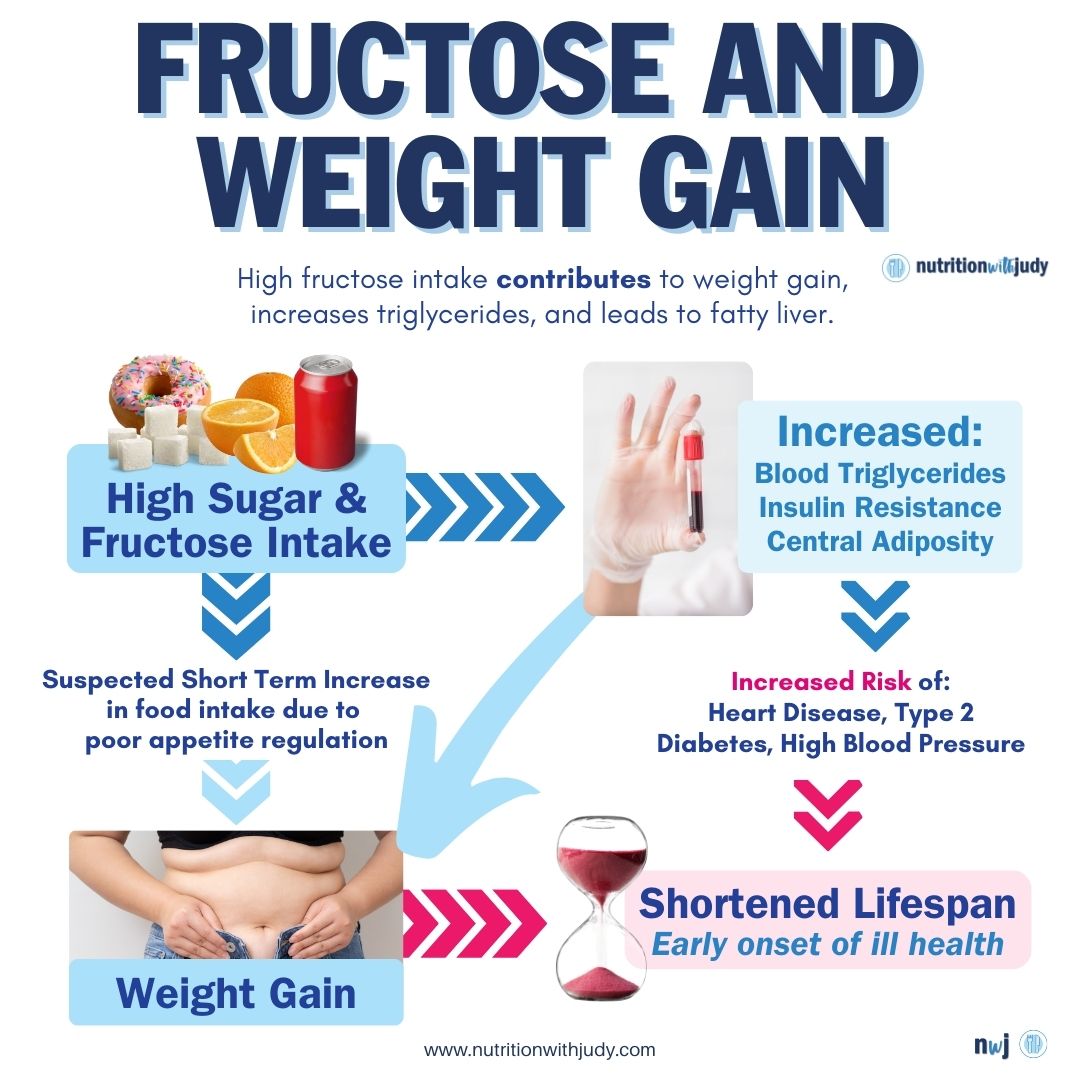
The truth is that the relationship between fructose and fatty liver needs thorough research as well as its comparison to alcohol. High intake of fructose contributes to weight gain, increases triglycerides, and leads to fatty liver.
Evidence confirms that high fructose intake contributes to the buildup of adipose (fat) tissue, obesity, systemic inflammation, oxidative stress, and insulin resistance. Excessive consumption of fructose participates in metabolic complications and affects the central nervous system. That’s why fructose intake may impair hunger and satiety control.
Indeed, fructose consumption can be one of many factors behind putting on a few pounds. This matters because being overweight or obese may contribute to fatty liver and other health concerns. What’s more, fatty liver is the most common liver-related problem observed in obese individuals. That happens because being overweight or obese is associated with increased consumption of calories. The excess calories contribute to the buildup of fat in the liver. The liver usually does a great job of processing and breaking down fats. Sometimes it’s unable to do so. When the liver doesn’t metabolize fats normally, too much fat builds up and may lead to fatty liver.
While it seems logical to adopt a leaner diet, one with less fat, to improve liver health, that’s not entirely a good idea. The best thing to do is to tackle the root cause of this problem. The root cause here is the excessive consumption of fructose. So, instead of fearing healthy fats that are actually good for you, it’s more practical to control fructose intake and make sure to limit it.
Fructose and Insulin Resistance in Fatty Liver
A review from the November 2002 issue of the American Journal of Clinical Nutrition reported that fructose consumption can contribute to insulin resistance syndrome. Since the production of leptin is regulated by insulin response to a meal, fructose intake lowers the circulating concentrations of the hormone leptin. Consumption of fructose may lead to insulin resistance, impaired tolerance to glucose, hyperinsulinemia, hypertension, and hypertriacylglycerolemia. This can also lead to weight gain.
Just like alcohol intake, fructose causes insulin resistance. Fatty liver may ensue. Insulin resistance contributes to the formation of fatty liver disease through the impaired ability of the hormone insulin to suppress lipolysis. As a result, people experience an increased delivery of free fatty acids to the liver.
Studies confirm that insulin resistance levels are high in patients with NAFLD and advanced fibrosis.
Fructose and Lipid Levels in Fatty Liver
Lipids are fatty substances that are a part of the cell membranes and help with moving and storing energy. There are two kinds of lipids in the body. They are cholesterol and triglycerides. Fructose consumption can increase both types of fats in the body. Dietary fructose at 20% of energy can elevate total cholesterol and low-density lipoprotein (LDL). A meta-analysis from The Journal of Nutrition also confirmed that a very high intake of fructose increased total cholesterol and LDL cholesterol levels.
High consumption of fructose is strongly associated with elevated dyslipidemia, high blood pressure, and insulin resistance. Excessive amounts of fructose enhance the accumulation of hepatic triglycerides. This can lead to fatty liver.
Through higher levels of cholesterol and triglycerides, fructose can contribute to fatty liver. It’s also useful to mention here that alcohol can also lead to higher levels of cholesterol and triglycerides. That’s why the carnivore diet stands out as a good way to avoid these problems. Since the carnivore diet relies on healthy animal fats and proteins and aims to avoid the consumption of carbs, including those from fruits, it reduces the risk of problems that high fructose intake could create.
Is It Safe to Eat Fruit On a Carnivore Diet?
Many people in the general population consume fructose regularly through fruit, foods containing fructose, or table sugar. High intake of fructose may cause serious health problems including fatty liver disease. For those who are adhering to carnivore or keto diets, avoidance of fructose aligns with these dietary principles. However, it’s important to understand how fructose works in the body and what could happen if you start consuming excessive amounts.
Based on the limited science available, we still believe that individuals who include fructose in their animal-based diets should be aware of the risks of fatty liver and high uric acid, and consider limiting their daily intake. While no existing studies are comparing the meat-only carnivore diet with an animal-based meat and fruit-only diet, some of the arguments from the meat + fruit community are suspect. We shared a newsletter debunking a lot of the research papers Paul Saladino uses to support his views of fructose. Many of the papers Saladino has shared were actually funded by Coca-Cola. Read more about the debunking here and some more of our thoughts on this here. Until significantly more clinical data and research are available regarding the role of fructose exclusively in fruit and NAFLD, we believe it’s best to err on the side of caution.
If you’re metabolically healthy, thriving on a meat-based diet with limited fruit, and your liver markers are normal, then we wouldn’t worry too much about including fructose in your diet. For individuals with chronic conditions, that aren’t metabolically healthy, who are overweight or obese, and/or struggle with sugar addiction, you may want to consider skipping fruit in your carnivore diet.
Work With Our Trusted Carnivore Diet Functional Nutritional Therapists
The Nutrition with Judy practice is honored to be a trusted carnivore diet practitioner support serving clients from around the globe. We’re passionate about helping our clients achieve root-cause healing in order to lead the best quality of life possible that’s nearly symptom-free. Our team is dedicated to educating our community about the incredible benefits of the carnivore diet. We welcome you to explore our free resources and are always available to support you through personalized protocols. Our Symptom Burden Assessment (SBA) is the perfect starting point for discovering your root cause and is required to work with our team— you can learn more in-depth about this powerful tool here.
Start your root-cause healing journey today and contact us any time with any questions or concerns.
DISCLAIMER: This content is for educational purposes only. While we are board-certified in holistic nutrition and are nutritional therapy practitioners, we are not providing medical advice. Whenever you start a new diet or protocol, always consult with your trusted practitioner first.



Dennis Cerletti
November 5, 2023 at 1:37 amIt would be nice to see how Dr Paul Saladino would show how 300 grams of fruit honey and dairy a day is no problem with causing fatty liver in a discussion with you.
Mark Wilson
November 5, 2023 at 2:59 amIt would be interesting to see research based upon fruit consumption rather than added fructose in drinks and processed foods. A quick scan through the evidence appears that most is based upon mixed diets and added fructose in foods and drinks rather than fruit. I’m interested that LDL=c is mentioned when the evidence for the dangers of raised LDL-c isn’t compelling, especially on an animal based diet. Interested to read your thoughts on this.
Krista Gutierrez
January 2, 2024 at 11:38 pmI am searching for how saturated fat can cause fatty liver. It was compared to fructose and possibly worse. Because I went to an animal-based diet I am worried. So far I cannot get anyone to address my question.